The COVID pandemic has mostly kept the flu out of sight, mind, and body. From June 2020 through March 2021, the U.S. Centers for Disease Control and Prevention (CDC) calculated that the emergency department visits for influenza accounted for less than 0.1% of all visits, which pales in comparison to the peaks of 3.1% in 2018 and 5% in 2019. In years past, as many as 1,150 people died weekly from respiratory viruses like flu and respiratory syncytial virus (RSV) without implementing emergency mitigation measures.
But as we re-emerge and reintegrate without the precautions to curb SARS-CoV-2, the flu (and RSV) likely will too.
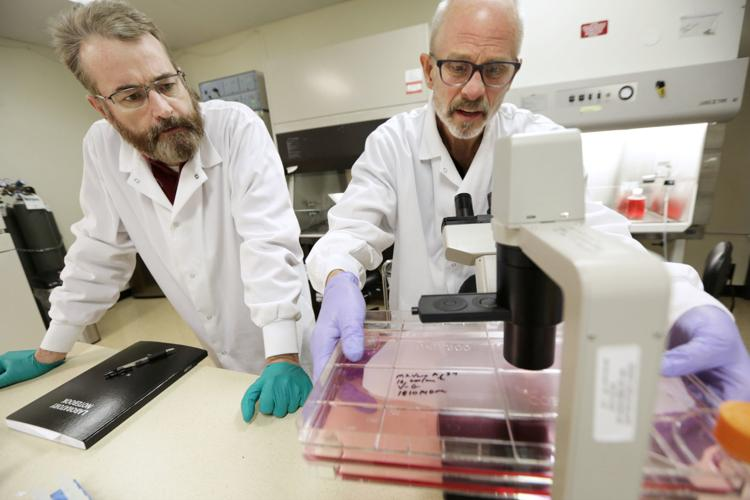
Based in Madison, WI, FluGen is a clinical-stage company transforming vaccine efficacy in respiratory diseases. The company’s lead candidate is M2SR—a live, single-replication, intranasal flu vaccine based on an invention by University of Wisconsin-Madison virologists and FluGen co-founders Yoshihiro Kawaoka, PhD, and Gabriele Neumann PhD.
In an unprecedented challenge trial, M2SR demonstrated protection against infection and illness across seven years of virus drift and induced a durable antibody response with the potential to cover an entire flu season and beyond. But M2SR has potential beyond the flu, showing activity as a vaccine vector for other respiratory vaccines and infectious diseases, including a COVID-19/flu combination.
GEN Edge spoke with founder, president, and CEO Paul Radspinner, to learn what sets FluGen’s flu vaccine apart from the competition and how the company plans to approach the global infectious disease market.
GEN Edge: How did FluGen get started?
Radspinner: I started the company with two world-renowned virologists out of UW Madison and the University of Tokyo back in 2008. We were driven to provide a more effective flu vaccine; we didn’t want to be one and done. The same approach that worked with polio is unrealistic for the flu—at least anything out there right now. Over the years, the approach to flu vaccines has been to take the antibody “hammer” out and hit it as hard as possible. The current flu vaccines are simply deadened versions of flu viruses injected into your arm. You get this amazing antibody response from these vaccines, and they do a great job at this one aspect of immunity. But what we know about the antibody response alone is that it’s not enough.
FluGen is driven to provide a more effective flu vaccine. We took a live flu virus and deleted a specific gene—the M2 gene—that created an opportunity for the virus to replicate but only once. Unlike FluMist—a cold-adapted attenuated live attenuated virus that replicates when you deliver it intranasally—we deliver ours intranasally with a single gene mutation or deletion that allows the virus to replicate a single time. That allows us to drive up the dose dramatically because there aren’t the high side effects you would get with a replicating virus.
This makes the vaccine more effective in two ways. First, we can get responses in all of the major immune effector systems. We’re hitting the antibodies. We’re also generating a mucosal response because we’re delivering intranasally, and then we’re getting a nice T-cell response, because we’re exposing people to all the flu proteins.
The other one is by fighting drift. As we didn’t have the flu last year because of COVID, vaccine producers were suddenly guessing what they were going to use. The vaccine may turn out to be 0% effective (it’s currently at 16%). If your bar isn’t higher than 50%, which the current vaccines have, you’re never going to do better. These currently marketed flu vaccines leave a lot to be desired at this point. This lack of efficacy can play into vaccine hesitancy where people doubt whether they should get the flu vaccine.. But we’ve shown that we get cross-reactive antibodies and protect against viral drift. So, we’re driven by good science that will provide protection across broad immune responses.
GEN Edge: How has government funding played a role for FluGen?
Radspinner: One of the challenges for a Midwest company is access to capital. We’ve been very efficient. We’ve raised about $50 million to date, but we’ve brought more than that in from NIH and the Department of Defense (DoD). We’ve been able to leverage those resources and get into Phase II. Now we’re into the stage where we must pursue big capital as we scale up substantially. We have to start doing more extensive clinical trials, which will be happening in the coming months and years.
There are multiple other resources as well. The Biomedical Advanced Research Development Agency (BARDA) is part of Health & Human Services (HHS) and was behind Operation Warp Speed. BARDA works on later-stage technologies, like the prevention of pandemics. BARDA is a group we would like to work with, where the strings that are attached are primarily getting the product to market. However we haven’t received BARDA funding yet.
The DOD group that’s funding us is called the Congressionally Directed Medical Research Programs (CDMRP) group, which came from some work that was done where Congress wanted to see more money going toward things like breast cancer research and development. Basically, Congress provides the budget and then helps focus on where the money will go. We’ve gone through this program for funding and they have been great to work with.
As it’s an internal granting mechanism, you have an internal panel that reviews it. With the CDMRP, if you are efficient, deliver results, and have ideas that look like they’re moving forward, they’re very interested in continuing to work with you. There’s a great deal of freedom there, as long as we stick to the rules. If you perform, what you find is that you tend to receive a positive reputation, which certainly doesn’t hurt you in the next round. But since these are all peer-reviewed grants, we don’t get funded if other scientists and clinicians don’t like it. There are no guarantees, but if you can get work done efficiently and get good results as we’ve done then you are more likely to be funded again. but it’s grant funding—it’s never guaranteed.
GEN Edge: What is FluGen’s manufacturing strategy?
Radspinner: The most capital-efficient way for us is to do manufacturing externally. We have a partner in France who is responsible for our current manufacturing. FluGen’s M2SR intranasal, single replication, influenza vaccine is manufactured in Vero cells modified to provide the M2 protein in trans back to the vaccine virus. This protein allows the vaccine to enter the cell but not to exit because M2SR does not carry the M2 gene.

GEN Edge: What other diseases does FluGen expect to tackle?
Radspinner: Half the time, it seems that investors want to invest in a single entity, that they’ll diversify their portfolio, and then other times they want a platform—it bounces back and forth. We have a platform, which is influenza as a vector. Work done years ago in the ‘60s showed that the flu is a very efficient vector. As the flu is very infectious, it makes a lot of sense. Maybe someday, COVID will be a vector because it’s pretty infectious. We’ve been able to add proteins for both COVID spike proteins into our flu vector. We’ve been able to work with RSV as well. We have IP in this area, and we see that there are multiple other areas that we could go into.
The only thing that limits us right now is time and capital. That’s what always limits companies like ours. But we are excited about the prospect of having data and being able to show what we can do. That’ll come later this year. One of the things that’s so beneficial about our system that is a shortcoming for most of the existing vaccines is that they don’t provide any protection at the site of infection. With COVID vaccines, you can be protected but can be infected and pass that on to other people. The reason is that you’re not getting any protection at the site of infection—the mouth nose and throat. Intranasal vaccines help to solve this problem.
GEN Edge: What are FluGen’s next steps?
Radspinner: We are moving from testing immunology, challenge studies, 200-250 subject studies to where we now have to move into larger clinical trials and manufacture larger lots. We have to start moving into the work that will lead to field studies—which, if you’ve watched COVID, can go as high as 50,000 subjects. In the coming years, I see us achieving those goals of manufacturing scale-up and of getting the vaccine into enough subjects to prepare us for field studies. Ideally we would be partnering with a company or companies that have the resources to do that kind of large-scale field study.
One of the challenges with existing vaccines is that their path to regulatory approval is simply with antibody responses. If you’ve seen the early data from mRNA vaccines on flu, you’ll notice that what they’re focused on is antibody response. They can get a quick approval based on antibody response alone. That doesn’t mean anything because it will not get you into the market. Nobody’s going to use that just because there’s an antibody response.
GEN Edge: How does FluGen plan to approach the international market?
Radspinner: Flu is a scourge that is a problem worldwide. Tens, if not hundreds, of thousands of people, die every year from flu. We would expect that as our vaccine goes through development, and if it is approved that it would be in the US, Europe, Japan, and all of the major markets. We hope we will be able to get into some of the other markets, which can be challenging. But I think that COVID has addressed that challenge to some degree. With COVID, vaccines have made it out to areas that we haven’t in the past. Hopefully, we’ll be able to take advantage of that as well.