Vaccines are among the hottest topics in biopharmaceuticals today. At the time of this article’s writing, 49.5% of the world’s population have already received at least one dose of a COVID-19 vaccine, and 26.65 million doses are being administered each day.1
The COVID-19 vaccines are a triumph, but they were almost somewhat expected—even though some commentators were predicting, as late as July 2020, that a COVID-19 vaccine could take years, or even decades, to develop.2 Looking back, we can appreciate that the vaccines were developed so quickly because of dramatic changes in vaccine production.
Several disruptive—but beneficial—changes in vaccine production were discussed at the 13th Annual Bioprocessing Summit, a virtual event that was held August 6–19, 2021. These changes are elaborated upon in this article, which presents insights gleaned from interviews between GEN and the vaccine production experts who delivered the Bioprocessing Summit’s most compelling presentations. These experts highlight the challenges of the pandemic, what we’ve learned, and—most important—what comes next.
Biotech’s poor relation
“Vaccines have been the poor relation of the biotech industry for 30 to 40 years,” says Lee Smith, PhD, principal consultant and managing director of biotech consultancy GreyRigge Associates. Big pharmaceutical companies, he explains, didn’t make enough profit to make vaccines a priority.
Traditional vaccine production followed a well-trodden path. “Initially, it was kind of a messy business where you would transfect eggs, purify and inactive viruses, and use them as vaccine,” recalls Henrik Ihre, PhD, strategic technology partnerships leader at Cytiva. Influenza vaccines, for example, were traditionally produced by harvesting viruses grown in embryonated hens’ eggs.3
More modern vaccines began relying on cell lines, from which viruses were produced and purified. The COVID-19 pandemic fast-tracked mRNA vaccines, which have been around—albeit in the form of theoretical constructs—for years.
“I think the first papers were published in the 1990s,” Ihre ventures. “They showed, in theory, that mRNA vaccines could work in animal models. Then, suddenly, the pandemic struck, and everyone was motivated to bring a vaccine to the market quickly.”
Exploiting a new vaccine platform
The mRNA platform technology has been validated by the pandemic, argues Zoltan Kis, PhD, a lecturer at the University of Sheffield. The mRNA platform technology is best known for the Moderna Spikevax and the Pfizer/BioNTech Comirnaty vaccines.4 Nonetheless, as Kis emphasizes, the mRNA platform technology is “disease agnostic—which is a huge advantage.”
The technology behind mRNA vaccines for COVID-19 is very novel, Kis continues. Unlike traditional vaccines, the Moderna and Pfizer jabs infect the recipient’s cells, causing them to produce antigens that resemble the COVID-19 spike protein.
As these vaccines were developed by genetically sequencing the COVID-19 spike protein, they’re very easy to adapt and change. “Viruses mutate all the time,” Ihre explains. “If they mutate so that the vaccine doesn’t work, it’s relatively easy to efficiently change the [mRNA] sequence—it’s almost a few clicks away on a computer.”
Moving to vaccine 2.0
Although the mRNA platform technology promises flexibility, it is still in its first iteration—and there is room for manufacturing improvements. “No templates exist for mRNA production,” points out Ratish Krishnan, associate director, Novel Modalities, BioProcessing Americas, MilliporeSigma. “The field faces significant challenges, such as developing the right processes, scaling up production to reach dose demands, addressing manufacturing bottlenecks, and complying with regulations.”
At Sheffield University, Kis is setting up a laboratory to research how to make mRNA production more efficient. One goal is to produce more mRNA vaccines while using smaller quantities of raw materials. Another goal is to make mRNA vaccines commercially using continuous production—a hot topic in the biotech sector.
Unlike traditional vaccine production, mRNA vaccine production doesn’t rely on cell lines. Consequently, as Kis argues, mRNA vaccine production is easier to transition into continuous mode. “The unit operations are very similar to those in conventional vaccine and biopharmaceutical production processes, but the reaction mix is simpler,” Kis details. So, the unit operations for mRNA vaccine production are simpler to transition from the outset.
Some of the unit operations are already continuous, he notes, such as encapsulating the mRNA in a lipid nanoparticle. “There are ways of making it a batch process,” he continues. “But keeping it continuous is easier.”
Kis is also using computer models to improve processes. He says that the models readily capture the simple reactions involving mRNA, and that the models be used to estimate quality attributes that can’t be measured in real time. “We’re developing soft sensors,” he reports. “They are computer models that infer quality attributes based on other parameters.”
One example is product degradation, which he says is more of an issue with mRNA vaccines than proteins or viruses. “Because mRNA vaccines degrade so easily,” he explains, “it’s important to ensure that they’re not doing so throughout the process.”
The challenges of mass production
Vaccine supply chains have been shaken up during the pandemic, and as a corollary, product formulation operations have been complicated. “The mRNA technology is very new,” Smith observes. “Maybe the formulation hasn’t caught up. In the case of the Pfizer/BioNTech vaccine, distributors need a specific cold chain to make sure the product doesn’t lose efficacy before being used.”
The pandemic has been a wake-up call about the logistics of pharmaceutical manufacturing, insists Jacob F. Kirkegaard, PhD, senior fellow at the Peterson Institute for International Economics (PIIE) and the German Marshall Fund (GMF). “Many companies,” he says “relied on subcontractors and took it for granted that the global logistics system would always deliver.” He adds that the sheer speed of vaccine development led to problems scaling up production and organizing supply chains, especially because the COVID-19 vaccines were first released when political pressure was high—in the deadly second wave.
According to Kirkegaard, Pfizer was relatively well positioned to cope with these problems. The company already had tremendous in-house production capacity. Moderna, he notes, was able to scale up and put together a supply chain from scratch with support from the U.S. government. Production and supply problems proved more pressing for AstraZeneca. The company, Kirkegaard says, didn’t have much production experience. Consequently, there were early shortages of AstraZeneca’s vaccine.
According to Smith, formulation and filling would have been an obstacle for any vaccine manufacturer in the United Kingdom. “When it came to producing the drug product, the United Kingdom,” he explains, “hadn’t invested in any vaccine commercial production or filling facilities for years.” Another problem, he says, was that the bioprocesses in AstraZeneca’s Belgium facility probably “fell over,” a setback he attributes to the facility’s “limited” experience coping with demands to greatly increase bioprocessing productivity. This caused vaccine shortages of “millions of doses” in Europe for around six weeks.
Lessons learned on formulation
The pandemic has prompted large pharmaceutical companies to simplify their supply chains and disperse production across multiple facilities. These efforts, Kirkegaard says, should reduce the risk of acute production shortages in future pandemics. Nonetheless, he adds, “We shouldn’t kid ourselves.”
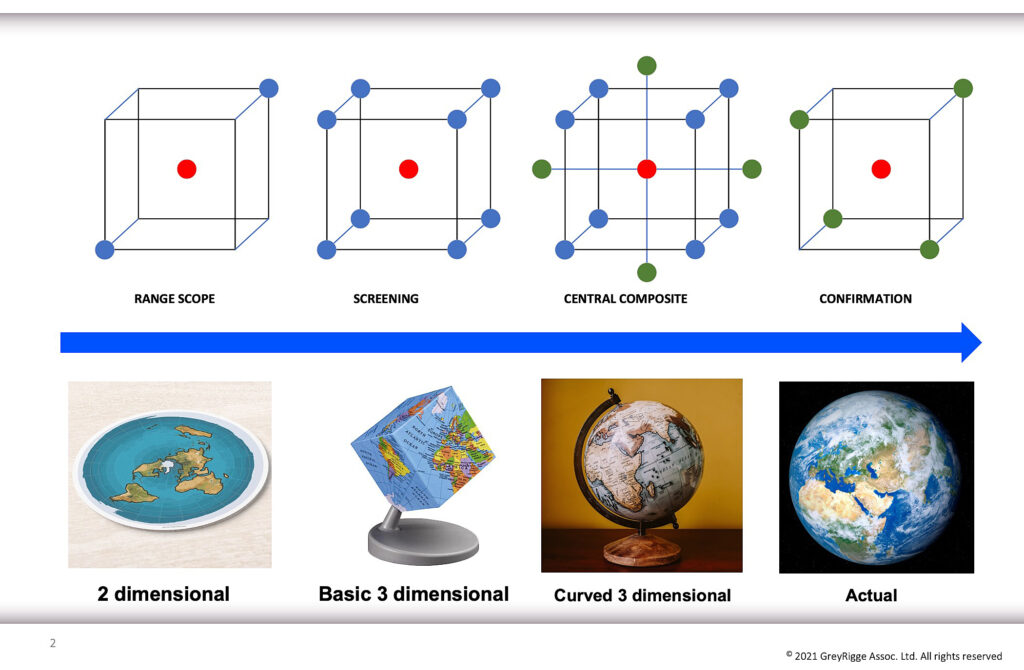
According to Smith, pharmaceutical companies also need to focus on making their bioprocesses more robust. He argues that these companies may operate too close to the edge of failure unless they adopt Design of Experiments methodologies. Another imperative is to adopt a formulation strategy that would make vaccines easier to supply and distribute.
“When it comes to formulations, they’ve been driven by what’s been done in the past,” he explains. “Formulators have tried to copy the formulations of old vaccines.” A better alternative would be to rely on data-driven approaches.
Widening the applications
Experts interviewed for this article felt that mRNA vaccines have now proven themselves, especially for pandemic flu-type situations where speed and versatility are key. However, there’s also the potential for the mRNA platform to be used in personalized medicine. For example, the platform could be used to produce personalized cancer vaccines.
“If a person gets cancer, you could do a biopsy of the tumor, look at all the proteins of the cancerous and nearby healthy tissue, and identify sequences found only in the tumor,” Ihre suggests. He adds that if you were to accomplish these tasks, you could create an mRNA vaccine targeting the cancerous proteins.
Each cancer vaccine would be tailor-made for a patient’s tumor, Ihre continues, and this would, in turn, change the production process. Among the likely changes are those in the types of raw materials required by manufacturers.
“There’s been a trend in the pandemic for fewer plasmids in larger quantities,” he says. “But for personalized cancer medicines, there will be a strong push for more different plasmids (used as templates in the manufacturing of desired mRNA sequences) at GMP-quality grade and smaller scale.”
Smith adds that the formulation challenges posed by cancer vaccines are fewer than those posed by mass production of mRNA vaccines. Many cancer vaccines aren’t expected to require ultra-low-temperature refrigeration. And even cancer vaccines that do wouldn’t call for expanded cold chain infrastructure. But Smith warns that formulation will remain a challenge for the future. “This probably won’t be the last pandemic we face,” he declares, “and the mRNA platform may not work for the next disease.”
References
- Our World in Data. Coronavirus (COVID-19) Vaccinations. Updated November 1, 2021. Accessed November 1, 2021.
- Colarossi N. How long it took to develop 12 other vaccines in history. Insider. Published July 18, 2020. Accessed November 1, 2021.
- Lee LYL, Izzard L, Hurt AC. A Review of DNA Vaccines Against Influenza. Front. Immunol. 2018; 9: 1568. DOI: 10.3389/fimmu.2018.01568.
- Bulik BS. Moderna locks up Spikevax name in Europe, joins Pfizer’s Comirnaty in wait for official brand approval in U.S. Fierce Pharma. Published June 303, 2021. Accessed November 1, 2021.

