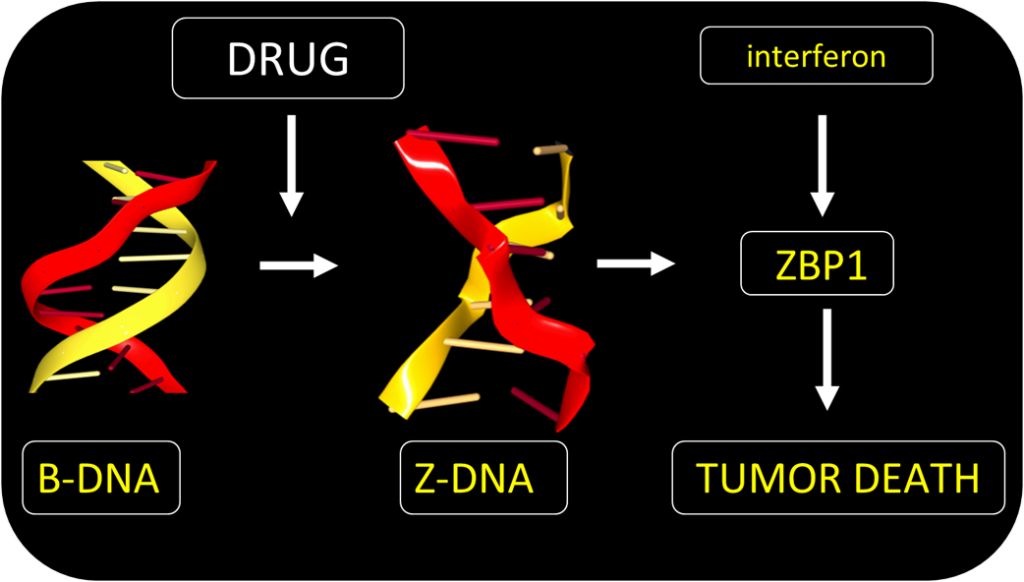
In a new study, scientists have identified a small molecule candidate drug that triggers the formation of left-handed Z-DNA in cells that in turn activates a highly immunogenic programmed pathway of inflammatory cell death called necroptosis in cancer-associated fibroblasts.
In studies on mice, the researchers showed that the compound (CBL0137), a member of the curaxin family, rekindles immune responses against melanoma resistant to immune checkpoint blockade (ICB)—an immunotherapy that boosts the patient’s own immune system to fight cancer—by mimicking influenza virus infections.
The findings were published in an article in the journal Nature titled, “ADAR1 masks the cancer immunotherapeutic promise of ZBP1-driven necroptosis.”
The paper resulted from an international collaboration led by Siddharth Balachandran, PhD, professor and co-leader of the blood cell development and function research program at Fox Chase Cancer Center in Philadelphia, and Alan Herbert, PhD, the founder of InsideOutBio, a Boston-based immune-oncology company currently operating in stealth mode. Computational studies were conducted by scientists at the Higher School of Economics led by Maria Poptsova, PhD with help from Carl Walkley, PhD, at the University of Melbourne, Yan Xu, PhD, from the University of Miyazaki, and Paul Thomas, PhD, from St. Jude Children’s Research Hospital.

Co-senior author of the paper, Balachandran, said, “We know that influenza viruses trigger very potent immune responses in infected cells. The entire immune system rushes to the site of infection and quickly eradicates the infected cells. We thought, ‘What if we could find a way to mimic a virus infection within a tumor that was otherwise cold?’ That way, the body’s own immune system will fight the tumor as if it were virally infected tissue.”
CBL0137 exploits Z-DNA—an alternative DNA conformation that twists to the left (unlike the standard right-handed Watson and Crick B-DNA)—that regulates immune responses to viruses. The response involves two Z-DNA binding proteins: the RNA-editing enzyme ADAR1 and the Z-RNA sensor ZBP1. Both ADAR1 and ZBP1 contain a domain that binds strongly to Z-DNA called the Zα domain which was discovered in earlier studies by Herbert, co-senior author of this study.

Herbert said, “It is a nice milestone in our understanding of how alternative DNA conformations, like Z-DNA, play an important role in human biology. The paper shows how basic research can lead to new and unexpected therapies. The process has taken a long time, starting with the initial discovery of the Zα domain and then the identification of Zα DNA variants that cause genetic diseases in humans. These discoveries validated a biological role for Z-DNA. The work now has led us to a new therapeutic approach for the treatment of cancer.”
Herbert added, “It is a pleasing turnaround given that the initial Z-DNA discoveries were widely dismissed by the scientific community as of little biological importance and further work was not ranked as worthy of funding by the National Institutes of Health peer review panels.”
Earlier studies by Balachandran’s lab and others, have shown the ADAR1 Zα domain turns off the immune response against normal “self” cells, while the ZBP1 Zα turns on immune response against virally infected cells. Tumors rely on ADAR1 to suppress cell death pathways that would otherwise kill tumor cells. Interactions between ADAR1 and ZBP1 decide whether a tumor cell lives or dies.
In the current study, the researchers administered CBL0137 directly into the tumor in mouse models of melanoma. This generated an antiviral response within the tumor, by inducing necroptosis and reversing unresponsiveness to ICB therapies in cancer-associated fibroblasts.
The team found CBL0137 bypasses ADAR1 suppression and directly activates tumor cell death by ZBP1. The drug acts regardless of the mutation that causes the cancer and kills fibroblasts supporting tumor growth. This enhances the effectiveness of ICB immunotherapy.
Balachandran said, “This is an important study for patients who have failed first-line immunotherapy because combining a ‘virus mimetic’ immune adjuvant with immunotherapy offers the opportunity to rekindle an immune response and make immunotherapy effective in otherwise unresponsive patients.”
The safety and dosing of CBL0137 as a standard chemotherapeutic has already been assessed in clinical trials.
“That’s a pretty big deal because there’s typically a multi-year gap between discovering a compound and using it in patients,” Balachandran said. “In this case, we can bypass that wait and get the compound directly into patients for combinatorial use with immunotherapy.”
This proposed Phase I clinical trial is slated to start later this year where CBL0137 will be administered with immunotherapy in patients with melanoma.