Researchers at the Brigham and Women’s Hospital and the Broad Institute report they have developed tissue-like structures in the laboratory to model barrier tissues, such as the intestines, to discover new targets for treatment. In a recent study, the researchers discovered a tissue-modifying molecule that can target intestinal stem cells and signal them to create Paneth cells, a rare but important cell type that can alter the gut microbiota. Previous studies have shown that Paneth cells are depleted in diseases such as inflammatory bowel disease and graft-versus-host disease. Replenishing these rare cells could represent a new therapeutic pathway. The team’s approach could also be used to identify molecules that could target other intestinal cell types.
Their findings are published in the journal Nature Biomedical Engineering, in an article titled, “Screening for modulators of the cellular composition of gut epithelia via organoid models of intestinal stem cell differentiation.”
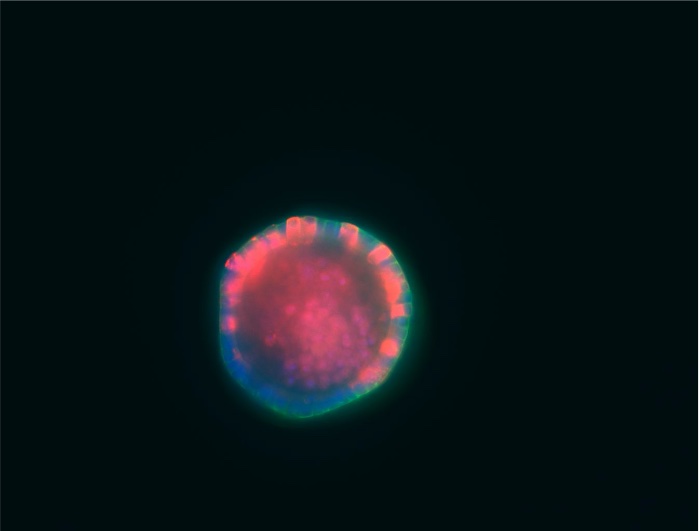
“The cellular composition of barrier epithelia is essential to organismal homeostasis. In particular, within the small intestine, adult stem cells establish tissue cellularity, and may provide a means to control the abundance and quality of specialized epithelial cells,” the researchers wrote.
“Yet, methods for the identification of biological targets regulating epithelial composition and function, and of small molecules modulating them, are lacking. Here we show that druggable biological targets and small-molecule regulators of intestinal stem cell differentiation can be identified via multiplexed phenotypic screening using thousands of miniaturized organoid models of intestinal stem cell differentiation into Paneth cells, and validated via longitudinal single-cell RNA-sequencing.
Their paper is the first approach to engineering barrier tissues by targeting and activating stem cells and causing new important cell types to form. “This could be used to potentially treat a wide range of diseases by manipulating the cell composition of the intestine,” said co-lead author Benjamin Mead, PhD, of the Broad Institute.
“This approach has wide-ranging implications and can be used to manipulate the cellular makeup of the intestine, including cells that can enhance barrier function, produce gut hormones, or that have key roles in coordinating insulin levels as well as food digestion and absorption,” said co-corresponding author Jeff Karp, PhD, distinguished chair in clinical anesthesiology, perioperative and pain medicine. “This approach also enables a completely new strategy to manipulate gut microbiota and thus offer insights into the treatment of a wide range of diseases.”