As people age they become more prone to blood clotting diseases, which can be caused when blood platelets clump together. This clumping can lead to strokes and cardiovascular disease. For decades, scientists have studied why older people’s blood cells behave in this way.
Studies in mice by researchers at the University of California, Santa Cruz (UCSC), and collaborators have now uncovered a distinct, secondary population of platelets that appears with aging. The researchers traced this population of platelets to its stem cell origins, and identified what they describe as the first-ever-discovered age-specific development pathway from a stem cell to a distinct mature platelet cell. The team found that these types of platelets display hyperreactive behavior and unique molecular properties, which could make them easier to target pharmacologically.
“The question for decades and decades has been: why are aging people at such high risk for excessive blood clotting, stroke, and cardiovascular disease?” said research lead Camilla Forsberg, PhD, UC Santa Cruz professor of biomolecular engineering. “We have this discovery of a whole new pathway that progressively appears with aging—troublemakers! That was never part of the discussion.”
The investigators reported on their studies in Cell, in a paper titled “An age-progressive platelet differentiation path from hematopoietic stem cells causes exacerbated thrombosis,” in which they concluded, “… our findings may profoundly impact the millions of elderly people at risk of experiencing adverse thrombotic events.”
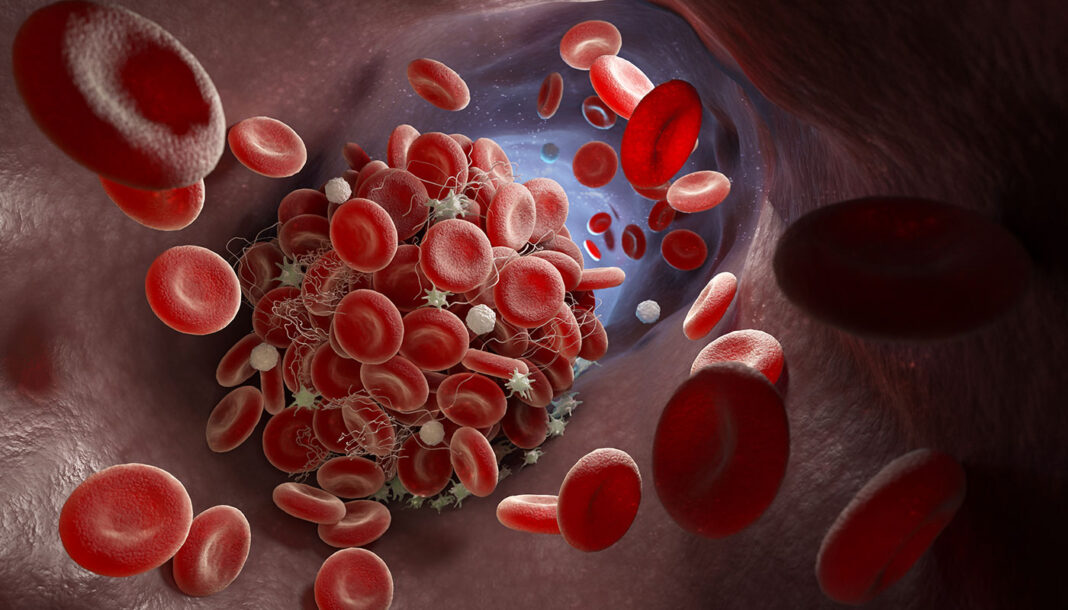
Red cells, white cells, and platelets (Plts) are the three types of blood cell produced by the body, the authors explained. Millions of platelets float around in the blood at all times, and their job, when an injury occurs either internally or externally, is to clot together to form a natural, living band aid. Platelet dysregulation, which is known to increase with age, occurs when these cells are either hyperreactive and form clots too often, or are under performing. Hyperreactivity is the much more widely seen problem, but both cases result in the body being unable to effectively manage bleeding and clotting. “Tipping the homeostatic balance toward inadequate Plt production is associated with higher risk for bleeding disorders, whereas Plt overproduction and hyper-reactivity lead to pathologic clot formation in thrombotic diseases such as deep vein thrombosis and ischemic stroke,” the authors stated.
All blood cells begin as a special type of stem cell known as hematopoietic stem cells (HSCs), and then mature through a series of intermediary steps that take them down a differentiation pathway that determines their fate as either platelets, red blood cells, or white blood cells. It’s been known for decades that hematopoietic stem cells decline with age, but that then presents scientists with a contradiction. If these hematopoietic cells are less healthy, why are the platelets they create hyperreactive? Moreover, the authors commented, “Although drastic increases in Plt dysregulation and adverse thrombotic events in aging populations have been clear for decades, distinct differentiation paths and cell populations have not been envisioned as underlying mechanisms of disease susceptibility upon aging.”
As stem cell biologists, the researchers at UC Santa Cruz traced the lineages of these stem cells in mouse models. They discovered that some platelets in aged animals did not follow the expected differentiation pathway. Instead, these platelets took what the UCSC researchers dubbed a “shortcut” pathway, skipping over the intermediary steps and immediately becoming megakaryocyte progenitors (MkPs), the blood cell stage immediately before platelet production. To the researchers’ knowledge, this is the first age-specific stem cell pathway ever discovered.
“… we employed the FlkSwitch model as a powerful tool for tracking hematopoietic differentiation pathways to demonstrate an unexpected cellular mechanism for the etiology of Plt-related disorders upon aging,” they stated. “The age-induced megakaryocyte progenitors have a profoundly enhanced capacity to engraft, expand, restore, and reconstitute platelets in situ and upon transplantation and produce an additional platelet population in old mice.”

The studies did not identify a trigger that might set off activation of this secondary pathway, but the investigators the results did indicate that it was not triggered by the aging environment itself. The scientists experiments showed that transferring a young hematopoietic stem cell into an aged environment did not trigger the shortcut pathway. And when an aged hematopoietic stem cell was put into young environment, the old stem cells continued to behave as old stem cells.
“That was surprising, the age resilience of the other pathway,” Forsberg said. “One of the platelet populations is not affected at all [by aging], whereas the one we have discovered is—so the whole phenomenon is not primarily induced by the environment, but by the differentiation path.”
Knowing that this secondary population of platelets exists will help scientists identify new ways to target and regulate these problematic cells via their stem cells. Researchers have not to date tried to target these upstream cells. “The emergence of Plt subpopulations during aging provides evidence that Plt heterogeneity is a determinant of age-related Plt diseases,” the scientists pointed out. “The production of mature cells via distinct differentiation paths offers a paradigm of stem cell aging that is currently unexplored.”
Poscablo said, “From our expertise, we can ask the questions of how to target the hematopoietic stem cell and now the megakaryocyte progenitor, which has never really been highlighted before as a place to target.”
Targeting these cells may not require the development of new drugs, but more simply inform the prescription of existing blood thinners, such as aspirin, which treat different patients to varying degrees even if they present with similar clotting-related symptoms. The researchers aim to use their mouse models to help identify which of the two populations of stem cells are more sensitive to aspirin and to other platelet drugs on the market. In the mouse models, they will also continue to study how to manipulate and control the shortcut pathway, with funding from the National Institutes of Health (NIH).
In parallel, and with the support of a grant from the California Institute for Regenerative Medicine (CIRM), the UCSC researchers are also working on finding this secondary population of platelets in humans. They concluded, “Our identification of the cellular origins and mechanisms of aging-enriched Plts provides compelling therapeutic opportunities for targeting HSCs and MkPs to control both Plt generation and functional reactivity throughout life.”