Myotonic dystrophy is one of the most common forms of muscular dystrophy. It is a genetic condition that causes progressive muscle weakness and wasting. No treatments currently exist that slow the progression of myotonic dystrophy, but symptomatic treatments are available. New research by scientists at the University of Rochester Medical Center (URMC) in animal models has identified the specific biological mechanism behind the muscle dysfunction found in myotonic dystrophy type 1 (DM1) and further shows that calcium channel blockers can reverse these symptoms.
Their findings are published in the Journal of Clinical Investigation in an article titled, “Verapamil mitigates chloride and calcium bi-channelopathy in a myotonic dystrophy mouse model.”
“DM1 involves misregulated alternative splicing for specific genes,” the researchers noted. “We used exon or nucleotide deletion to mimic altered splicing of genes central to muscle excitation-contraction coupling in mice. Mice with forced skipping of exon 29 in the CaV1.1 calcium channel combined with loss of ClC-1 chloride channel function displayed markedly reduced lifespan, whereas other combinations of splicing mimics did not affect survival. The Ca2+/Cl– bi-channelopathy mice exhibited myotonia, weakness, and impairment of mobility and respiration. Chronic administration of the calcium channel blocker verapamil rescued survival and improved force generation, myotonia, and respiratory function.”
“The main finding of our study is that combined calcium and chloride channelopathy is highly deleterious and plays a central role in the function impairment of muscle found in the disease,” said John Lueck, PhD, lead author and an assistant professor at URMC in the departments of pharmacology and physiology, and neurology. “Our research also suggests that muscle impairment in DM1 is potentially mitigated by common clinically available calcium channel blockers and that calcium channel modulation is a potential therapeutic strategy.”
More than 20 years ago, URMC neurologist Charles Thornton, MD, and others uncovered how a genetic flaw—a “stutter” that results in thousands of repetitions of code on a segment of chromosome 19—gives rise to DM1. This repeat expansion, which grows longer over time, results in the creation of abnormal RNA which accumulates in the nucleus of cells and affects the normal processing of many other RNAs.
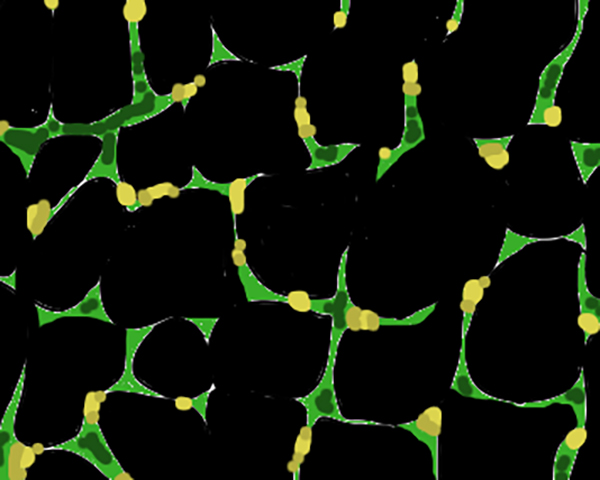
This toxic RNA specifically disrupts the function of muscleblind-like (MBNL) proteins responsible for regulating the splicing of transcripts important for maintaining healthy muscle function. Among other things, these splicing defects impair the function of receptors for calcium and chloride channels, gateways in muscle cells that help convert electrical signals from motor neurons into chemical signals within the muscle cells.
“Myotonic dystrophy is a really complicated disorder, which you can think of as almost like an aggregate of many diseases,” said Lueck. To accomplish this, the team created a mouse model that mimicked four of the splicing defects found in DM1 in genes associated with the calcium and chloride channels. These mice exhibited severe myotonia, muscle weakness, impaired mobility, respiratory defects, and a marked reduction in lifespan.
The involvement of the calcium channel in muscle dysfunction presented an opportunity and a target. When the team treated the mice with verapamil, a calcium channel blocker used to treat hypertension and chest pains, the mice quickly recovered muscle function and began to resemble their healthy, wild-type peers. The findings were possible by years of close observation of the animals by Lily Cisco, a graduate student in the Lueck lab who is first author of the study.
The researchers have emphasized that verapamil is not an appropriate treatment for DM1 in humans due to its potential cardiac side effects. “We think that the calcium channel is a new therapeutic target and if we can target it correctly, pharmacologically that it will improve muscle function and health. Our goal now is to find the appropriate and safe calcium channel blocker that will do the job and we believe it exists.”