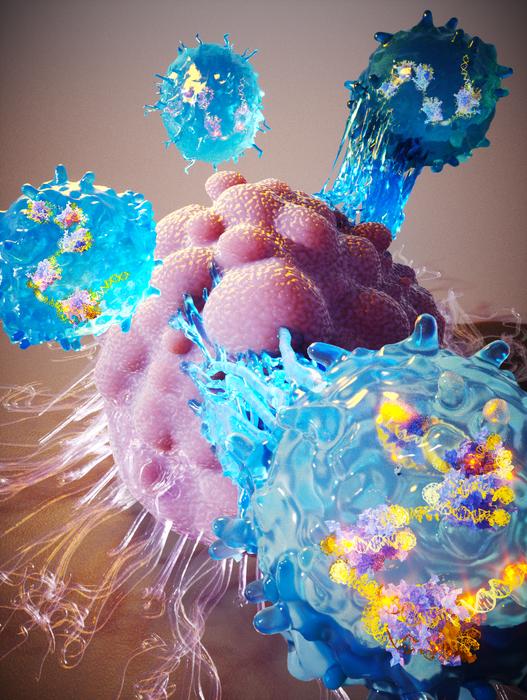
Researchers at Duke University have adapted CRISPR technologies to enable high-throughput screening of gene function in human immune cells, and discovered that a single master regulator of the genome can be used to reprogram a network of thousands of genes in T cells and greatly enhance cancer cell killing.
The master regulator transcription factor (TF) gene is called BATF3 and is one of several genes that the researchers identified and tested for improving T cell therapies. These targets, and the methods developed to identify, test, and manipulate them, could make any of the T-cell cancer therapies currently in use and under development more potent. Combined with other advances, the platform could also enable generalized, off-the-shelf versions of the therapy and expansion into other disease areas such as autoimmune disorders.
“A known barrier to using T cells to fight cancer is that they tend to get ‘tired’ over time and lose their ability to kill cancer cells,” said Sean McCutcheon, who is co-lead author of the team’s published paper in Nature Genetics. “We’re identifying manipulations that make T cells stronger and more resilient by mimicking naturally occurring cell states that work well in clinical products.”
McCutcheon, together with research lead Charles Gersbach, PhD, the John W. Strohbehn distinguished professor of biomedical engineering at Duke, and colleagues, reported on their findings in a paper titled, “Transcriptional and epigenetic regulators of human CD8+ T cell function identified through orthogonal CRISPR screens.”
T-cell therapy is a decade-old approach to treating cancer. More recent approaches involve reprogramming immune system cells to seek and destroy cancerous cells that they might otherwise overlook. Many companies are working to enhance the technology, mostly through the use of genetic engineering techniques that instruct the T cells how to identify cancerous cells and make them more effective at destroying them. “Adoptive T-cell therapy (ACT) holds tremendous potential for cancer treatment by redirecting T cells to cancer cells via expression of engineered receptors that recognize and bind to tumor-associated antigens,” the authors noted.
There are currently six FDA-approved T-cell therapies for specific leukemias, lymphomas, and multiple myeloma. Such approaches and treatments, however, do not currently fare well when applied to solid tumors, although there are hints of success in certain studies. Solid tumors often present large physical barriers for the T cells to overcome, and the sheer number and density of cancer cells presenting targets can lead to T-cell exhaustion, whereby the cells are no longer able to mount an antitumor response.
“In some cases, T-cell therapy works like a miracle drug, but in most others, it hardly works at all,” said Gersbach. “We are looking for generic solutions that can make these cells better across the board by reprogramming their gene regulation software, rather than rewriting or damaging their genetic hardware.”
Gersbach and his laboratory have spent the past several years developing a method that uses a version of the gene-editing technology CRISPR-Cas9 to explore and modulate genes without cutting them. Instead, it makes changes to the structures that package and store the DNA, affecting the activity level of the accompanying genes.
McCutcheon, a PhD candidate working in Gersbach’s lab, focused on regions of this “dark genome” that change as T cells transition between states, such as functional versus exhausted. “Here we developed pooled, epigenetic CRISPR screening approaches to systematically profile the effects of activating or repressing 120 transcriptional and epigenetic regulators on human CD8+ T cell state,” the investigators commented. Through their screen the researchers identified 120 genes that encode “master regulators,” which are responsible for the activity levels of many other genes. Using the CRISPR platform, the researchers dialed the activity levels of these targets both up and down to see how they affected other known markers of T-cell function.
While several promising gene candidates emerged, one of the most promising was a gene called BATF3. When McCutcheon subsequently delivered BATF3 directly to the T cells, there were thousands of tweaks to the packaging structure of the T cells’ DNA, and this correlated with increased potency and resistance to exhaustion. “We found that BATF3 overexpression promoted specific features of memory T cells and attenuated gene programs associated with cytotoxicity, regulatory T cell function, and exhaustion,” they wrote. “Upon chronic antigen stimulation, BATF3 overexpression countered phenotypic and epigenetic signatures of T-cell exhaustion.”
The researchers put BATF3 through a battery of tests. The most interesting results came when they overexpressed BATF3 in T cells programmed to attack human breast cancer tumors in a mouse model. While the standard-of-care T-cell therapy struggled to slow tumor growth, the exact same dose of T cells engineered with BATF3 completely eradicated the tumors. “BATF3 enhanced the potency of CAR T cells in both in vitro and in vivo tumor models and programmed a transcriptional profile that correlates with positive clinical response to adoptive T cell therapy,” they commented.
While the results with BATF3 are promising, the team is even more enthusiastic about the general success of the methodology to identify and modulate master regulators to improve therapeutic performance, which they have been developing for the better part of a decade.
Researchers can now readily profile master regulators of T cell fitness using any T cell source or cancer model and under various experimental conditions that mimic the clinical setting. “This demonstration is a crucial step toward overcoming a major hurdle to getting T cell therapy to work in more patients across a greater range of cancer types,” Gersbach noted.
For the last part of the reported study, McCutcheon screened T cells, with or without BATF3, while using CRISPR to remove every other master regulator of gene expression—more than 1,600 regulators in total. “… we performed CRISPR knockout screens that defined cofactors and downstream mediators of the BATF3 gene network,” the authors stated. This led to the discovery of a whole new set of factors that could be targeted alone or in combination with BATF3 to increase the potency of T-cell therapy. “Overall, this work expands the toolkit of epigenome editors and our understanding of regulators of CD8+ T cell state and function. This catalog of genes could serve as a basis for engineering the next generation of cancer immunotherapies,” they noted.
“This study focused in depth on one particular target identified by these CRISPR screens, but now that Sean and the team have the whole discovery engine up and running, we can do this over and over again for different models and tumor types,” Gersbach said. “This study suggests many strategies for applying this approach to enhance T-cell therapy, from using a patient’s own T cells to having a bank of generalized T cells for a wide variety of cancers. We hope that these technologies can be generally applicable across all strategies.”