Researchers at the Institute of Molecular Biotechnology (IMBA) of the Austrian Academy of Sciences, and at ETH Zurich have developed a novel single-cell brain organoid screening system to help identify the gene mutations, vulnerable cell types, and gene regulatory networks that underlie autism spectrum disorders (ASDs). The new system, called CRISPR–human organoids–single-cell RNA sequencing (CHOOSE), combines brain organoid technology with CRISPR-based genetic targeting, allowing scientists to comprehensively test the effects of multiple mutations in parallel, at a single-cell level within human brain organoids.
The researchers say their new technique offers unparalleled insights into ASD, which is one of the most complex human brain disorders, and has implications that could offer hope for clinical research. The CHOOSE system is also transferable to the study of other disease fields, suggested research lead Jürgen Knoblich, PhD, IMBA scientific director. “We anticipate that our technique will be widely applied beyond brain organoids to study various disease-associated genes.” Knoblich is co-corresponding author of the team’s published paper in Nature, which is titled, “Single-cell brain organoid screening identifies developmental defects in autism.” In their paper, the team concluded, “By employing a pooled CRISPR screening system in conjunction with validation, our study provides a developmental and cell type-specific phenotypic database for ASD gene loss-of-function research.”
Human brain development relies on processes that are unique to humans, allowing us to build an intricately layered and connected cortex. However, the exact mechanisms and pathways aren’t yet fully understood, the authors suggested. “These processes are governed by precise and highly orchestrated genetic and molecular programs, many of which have remained elusive.” These unique processes in human brain development also make neurodevelopmental disorders more likely in humans. As an example, many genes conferring a high risk of developing autism spectrum disorder are crucial for cortex development. And while clinical studies have shown causality between multiple genetic mutations and autism, researchers still do not understand how these mutations lead to brain developmental defects and neurodevelopmental disorders (NDDs). Further, the investigators pointed out, “… many NDDs, such as autism spectrum disorder (ASD), are diagnosed only after birth, when brain development is almost complete … Analyzing the developmental and cell type-specific defects associated with ASD in a human context is crucial but is often constrained to neuroimaging and postmortem tissue studies.” And because of the uniqueness of human brain development, animal models are of limited use. “Only a human model of the brain can recapitulate the complexity and particularities of the human brain,” said Knoblich.
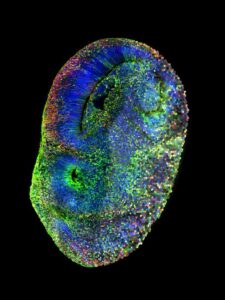
Researchers in the IMBA lab of Knoblich, and the ETH Zurich lab of Barbara Treutlein, PhD, developed a technique to screen a complete set of key transcriptional regulator genes linked to autism. This development is especially impactful since the genes of interest can be examined simultaneously within a single mosaic organoid, unlocking the ability to carry out intricate, efficient, and expedient genetic screening in human tissue.
In the CHOOSE system, each cell in the organoid carries at most one mutation in a specific ASD gene. This makes it possible to trace each mutation’s effect at a single-cell level and map each cell’s developmental trajectory. “With this high-throughput methodology, we can systematically inactivate a list of disease-causing genes,” said study first and co-corresponding author Chong Li, PhD, a postdoctoral fellow in the Knoblich group. “As the organoids carrying these mutations grow, we analyze the effect of each mutation on the development of each cell type.”
Using the CHOOSE system, the researchers showed that mutations in 36 genes known to put carriers at high risk of autism lead to specific cell type changes in the developing human brain. They identified critical transcriptional changes regulated through common gene regulatory networks, or GRNs. “Using single-cell multiomic data, we construct a developmental gene regulatory network (GRN) of cerebral organoids and identify ASD-enriched regulatory hubs connected to the genes that are dysregulated in response to genetic perturbations,” they wrote. A GRN is a set of molecular regulators that interact with each other to control a specific cell function, explained Li. “We demonstrated that some cell types are more susceptible than others during brain development and identified the networks that are most vulnerable to autism mutations.”
“With this approach, we learned that autism-causing genes share some common molecular mechanisms,” added Knoblich. Yet, these common mechanisms can lead to markedly distinct effects in different cell types. “Some cell types are more vulnerable to mutations that lead to autism, especially some neural progenitors—the founder cells that generate neurons. This is true to the point that the pathology of autism could already emerge early during brain development. This indicates that some cell types will necessitate more attention in the future when studying autism genes,” commented Li.
Among the 36 genes, perturbations to a gene known as ARIDIB were found to be of particular significance. To confirm whether their findings were relevant to human disorders, the researchers teamed up with clinicians from the Medical University of Vienna and generated brain organoids from stem cell samples derived from two different patients with ARIDIB mutations. “Among the 36 genes, one of the most significant changes in cell type composition was identified in the context of ARID1B,” the team commented. “Specifically, perturbing ARID1B expands ventral radial glia cells and increases their transition to early oligodendrocyte precursor cells (OPCs), a phenotype we verify in brain organoids generated from ARID1B patient-derived induced pluripotent stem cell (iPS cell) lines.” Koblich added, “The organoids generated from both patients showed marked developmental defects linked to a specific cell type. We could validate these in vitro observations by comparing the organoid structures to the prenatal MRIs of one of the patients’ brains.” This finding indicated that the organoid data closely matched clinical observations.
Mutating several genes in parallel and tracking their effects generates an enormous amount of data. To analyze this complex dataset, co-corresponding author Treutlein and her team at ETH Zurich used quantitative bioinformatics and machine learning approaches. “Using this high-throughput single-cell expression data, we can quantify whether a given cell type is more or less abundant due to a given mutation, and we can also identify sets of genes that are commonly or distinctly affected by each mutation. By comparing across all the gene mutations, we can reconstruct the phenotypic landscape of these disease-linked genetic perturbations,” explained Treutlein.
The CHOOSE system represents a major advance in research on disease-causing genes, giving scientists access to a versatile and high-throughput method that can be applied to any disease and in any human model system, the investigators suggested. Importantly, CHOOSE considerably speeds up the analysis in comparison to traditional genetic loss-of-function approaches. “We can see the consequence of every mutation in one experiment, thus shortening the analysis time drastically when compared to traditional methods, using an approach that for decades was only possible in organisms like the fruit fly,” explained Knoblich. “Additionally, we can still benefit from a hundred years of scientific literature about disease-causing genes.”
The authors noted, “The combination of high-content perturbation screening and validation in a patient-specific context exemplifies the effectiveness of employing organoid systems to study NDDs.” While noting the limitations of their reported study, the researchers suggested, “The ability to determine cell type-specific contributions to genetic disorders in a systematic, scalable, and efficient manner will greatly enhance our understanding of disease mechanisms.”
In addition to gaining unparalleled insights into the pathology of autism, the team underlines the versatility and transferability of the CHOOSE system, which gives scientists and clinicians a robust and precisely controlled high-throughput screening tool that considerably shortens analysis time and provides invaluable insights into disease mechanisms.
As the authors concluded, “Our study paves the way for high-throughput phenotypic characterization of disease susceptibility genes in organoid models with cell state, molecular pathway, and gene regulatory network readouts … As the CHOOSE system provides a robust, precisely controlled screening strategy, we anticipate that it will be widely applied beyond brain organoids to study disease-associated genes.”


