A study by researchers at the University of Michigan Rogel Cancer Center suggests that androgen receptor (AR) inhibitor drugs, such as enzalutamide (enza) can fundamentally rewire and reshape how prostate tumors function, and in certain cases even make them more aggressive. The team carried out gene expression profiling of biopsies of metastatic castration-resistant prostate cancer (CRPC) from men prior to treatment using enza, and also at progression. Their analyses indicated evidence of lineage plasticity, and also identified a gene signature, which they have yet to validate, associated with a risk of therapy-induced lineage plasticity and poor patient survival.
The study was led by Joshi Alumkal, MD, Wicha Family Professor of Oncology and Professor of Internal Medicine at the Rogel Cancer Center, in collaboration with the lab of Zheng Xia, PhD, at the Oregon Health & Sciences University Knight Cancer Institute. Alumkal told GEN, “Our results demonstrate that in approximately 15% of cases, tumor lose reliance on the original target of the drug enzalutamide—the androgen receptor. Our results also suggest there may be baseline gene expression changes that allow one to predict that this deadly form of resistance called lineage plasticity, or differentiation change, may happen with enzalutamide treatment.”
The researchers reported their findings in Nature Communications, in a paper titled “Transcriptional profiling of matched patient biopsies clarifies molecular determinants of enzalutamide-induced lineage plasticity.” Thomas Westbrook, MD, hematology-oncology fellow, was the study’s co-first author, along with postdoctoral fellow Xiangnan Guan, PhD.
Androgen receptor signalling inhibitor (ARSI) drugs such as enzalutamide block male hormones from activating the androgen receptor, and have been used to treat advanced prostate cancer for more than a decade. “The androgen receptor (AR) signaling inhibitor enzalutamide (enza) is one of the principal treatments for metastatic castration-resistant prostate cancer (CRPC),” the authors wrote. But such drugs can eventually stop working, and “progression to castration-resistant prostate cancer (CRPC) is nearly universal,” the team continued.
So while Enza improves progression-free survival and overall survival in patients with CRPC, and also increases overall survival in patients with hormone-naïve prostate cancer who are starting androgen deprivation therapy (ADT) for the first time, “… one third of patients do not respond, and those with de novo resistance have a slightly increased risk of death compared to responders,” the scientists noted. And despite significant study, clinical enza resistance remains poorly understood.
“Resistance to targeted therapies is nearly universal in cancer treatment,” Alumkal commented to GEN. “However, there is an incomplete understanding of resistance mechanisms for most cancer therapies due to the paucity of data utilizing matched biopsies from patients treated with these agents. For patients with prostate cancer, androgen deprivation therapy with drugs like the androgen receptor (AR) inhibitor enzalutamide (enza) is the principal treatment approach, but much remains unknown about how this drug stops working.”
Male hormones function as fuel, turning on the androgen receptor that acts as the engine of prostate cancer cells. For the past 80 years, treatment for patients with advanced prostate cancer has focused on interfering with these hormone levels—now typically done through hormone lowering treatments, and drugs like enzalutamide. Eventually, however, nearly all tumors develop workarounds and escape treatment, and in most cases, tumors remain dependent on male hormones to power their growth. Other examples of treatment resistance remain poorly understood.
“The greatest unmet need in the clinic right now is understanding the workarounds in a tumor that becomes resistant to androgen receptor targeting drugs so we can determine how best to treat the patient whose tumor has begun to grow,” said Alumkal, “Once enzalutamide stops working, there are limited options. We don’t know how or why most tumors become resistant.”
The investigators wanted to understand what was present in these tumors to begin with— prior to therapy—and what happened after tumors started to grow during enzalutamide treatment, to help them understand the workarounds in tumors from individual patients. “… we hypothesized that comparing gene expression profiles between matched CRPC tumor biopsy samples prior to enza and at the time of progression would identify pre-treatment and treatment-induced resistance mechanisms in individual patients,” they explained. To do this the team recruited patients to a longitudinal study to obtain metastatic biopsies before enzalutamide treatment and at the time the tumor became resistant to treatment. Serial biopsies were collected from 21 patients.
Alumkal says this is the largest collection of matched metastatic biopsies before and after enzalutamide. “To understand resistance to drugs, researchers often collect samples from some patients before treatment and from a different group of patients whose tumors are treatment resistant,” he said. “However, that approach is much less precise because there could be other significant differences between those patients. You can’t pinpoint if the differences have anything to do with drug exposure or have more to do with the tumors just being different to begin with.”

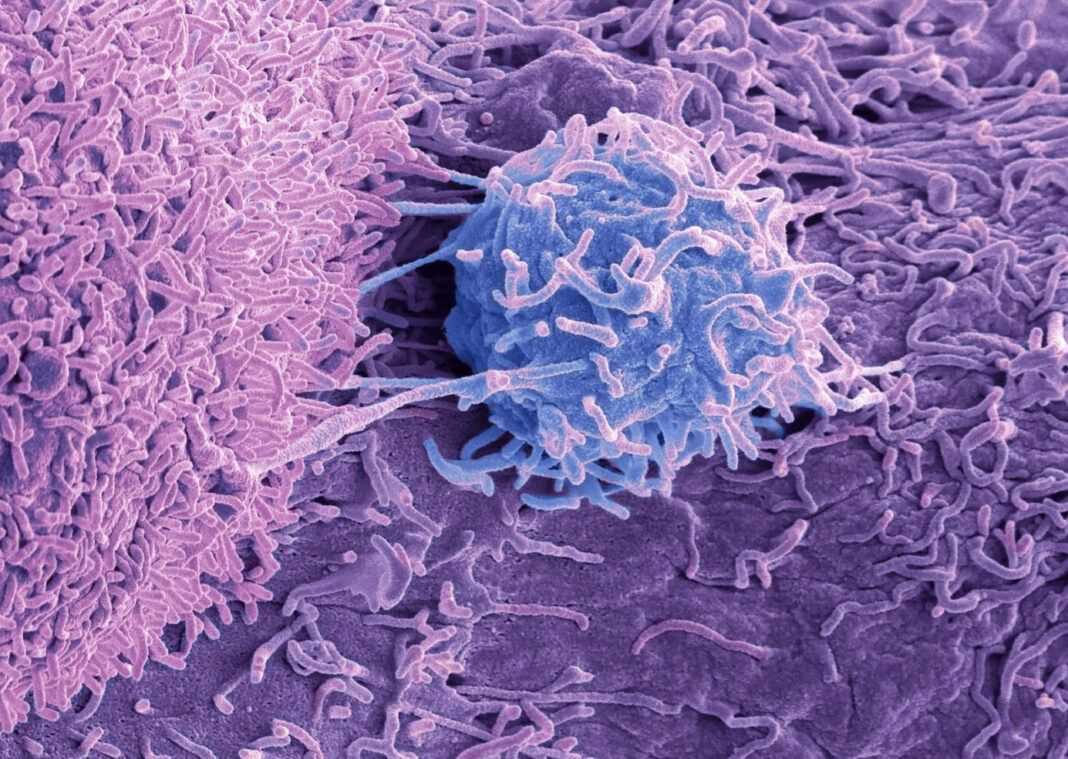
The sequential sampling approach provided a much clearer picture of how enzalutamide resistance might emerge. “Metastatic biopsies are not routinely done in clinical practice, but performing these biopsies before and after treatment was essential for us to understand how tumors were changing after enzalutamide treatment,” Alumkal further explained to GEN. “We used laser capture microdissection to enrich for tumor cells prior to RNA-sequencing. We also performed DNA-sequencing and multiplex immunofluorescence. The latter enabled us to understand the heterogeneity of the tumors at baseline and progression.”
When the researchers compared the baseline sample to the progression sample from the same patient, most tumors showed no significant gene expression changes. “We determined that most progression tumors clustered with their baseline pair and that most tumors did not change their transcriptional cluster designation between baseline and progression,” the authors wrote. “Many patients’ matched tumors expressed a similar gene expression program, regardless of whether a different lesion or tissue type was biopsied, suggesting homogeneity of many lesions within the same patient.”
Alumkal stated, “That the gene expression program of a tumor prior to treatment looked very similar at progression while on enzalutamide is quite remarkable. It speaks to how well most of the tumors were able to adapt and keep the androgen receptor engine on despite enzalutamide treatment.”
But that wasn’t the only surprise. In three of the 21 cases, Alumkal and his team saw a profound shift in tumor gene expression profile. “We knew that sometimes tumors become fuel-independent and no longer rely on the androgen receptor,” he said. “These tumors instead turn on a gene expression program more common in nerve cells, rather than prostate cells, and shift to an aggressive form called neuroendocrine prostate cancer.”
But the researchers found that in these 15% of cases the tumors also became fuel-independent for another reason. Alumkal said, “These tumors were wired in a unique way and were most consistent with a subtype of prostate cancer called double-negative prostate cancer (DNPC), meaning the tumors no longer had the androgen receptor as an engine. But they also did not become neuroendocrine prostate cancer.”
He used an analogy of vehicles and how they are powered, to describe this change. “Initially, nearly all prostate tumors are gas guzzlers: very fuel dependent and powered by the androgen receptor as the engine. When treated with hormonal treatments, most tumors remain fuel-dependent but become more fuel efficient, able to go farther with less gasoline. “Our work showed that the majority of the tumors—even after receiving enzalutamide—remain very fuel-dependent, which suggests that continuing to target the androgen receptor could make an enormous difference in these tumors.”
Alumkal suggested that three tumors converted to become double negative prostate cancer—akin to an electric vehicle. “We identified three baseline tumors that may have been in an intermediate state at high risk of lineage plasticity,” the scientists wrote. “In each case, these patients’ progression biopsies underwent significant transcriptional changes—changing from ARPC [androgen receptor-driven prostate cancer] to DNPC/Aggarwal cluster 2 at progression.”
Results from the sequential sampling method suggest that enzalutamide is causing tumors to adapt, in some cases dramatically. “The gasoline engine was replaced by a completely distinct set of machinery that allowed tumors to grow and survive,” Alumkal said. “The DNA mutations found in the baseline and progression biopsies from these converter tumors were the same, which strongly suggests that enzalutamide completely rewired the engine of the original fuel-dependent tumor to become fuel-independent at disease progression. “It’s a dramatic shift to wrap your head around.”
Although the baseline tumors appeared similar under the microscope, the researchers identified specific genes that were highly expressed in those that eventually became double negative prostate cancer. “We identified a signature of 14 genes highly upregulated in base line tumors from the converters,” they wrote. This results suggest that certain tumors exist in a hybrid state, initially dependent on fuel but at risk for becoming a fuel-independent double negative prostate cancer during enzalutamide treatment.
Alumkal acknowledged that the gene signature identified is a preliminary finding, and the team has more work to do. “We are not aware of any published datasets that include matched biopsies with RNA-sequencing and information on change in tumor phenotype,” the researchers noted. “Therefore, it was not possible to validate the predictive ability of this signature of lineage plasticity risk.” However, they noted, “… high activity of this signature in two independent cohorts was associated with poor overall survival after ARSI treatment.”
“Still, the fact that the DNA looks similar in the converters strongly indicates that enzalutamide is reprogramming tumors,” Alumkal stated. We have more work to do, but it may be possible up-front to identify patients at greatest risk of having their tumor become fuel-independent after treatment with drugs like enzalutamide.”
As he further explained to GEN, “Our results demonstrate that in approximately 15% of cases, tumor lose reliance on the original target of the drug enzalutamide—the androgen receptor. Our results also suggest there may be baseline gene expression changes that allow one to predict that this deadly form of resistance called lineage plasticity, or differentiation change, may happen with enzalutamide treatment. A natural next step from this work is a more careful dissection of mechanisms that contribute to lineage plasticity risk, including chromatin or microenvironmental contributors. Furthermore, it will be important to attempt to validate the lineage plasticity risk signature we identified in additional independent cohorts with matched biopsies. Once biomarkers of lineage plasticity risk are identified, prospective clinical trials testing drugs that target pathways highly activated in these tumors may be warranted.”
Pointing out the strengths and limitations of their study, the authors also stated in their paper, “In the future, identifying biomarkers for those whose tumors are at greatest risk of undergoing lineage plasticity vs. those whose tumors are most likely to remain AR-driven may facilitate development of up-front combination clinical trials testing drugs predicted to block these two principal enza resistance mechanisms.”