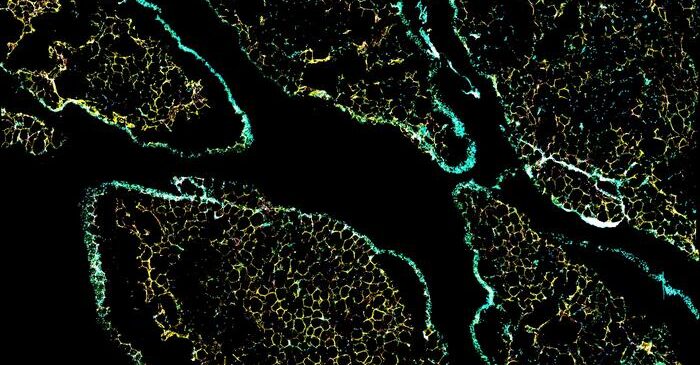
Adipose tissue is a cellular mosaic. To make sense of it—and gain a better understanding of metabolic conditions such as obesity—the different tiles need to be distinguished, no matter how alike they may seem. That’s why scientists at the Swiss Federal Institute of Technology in Lausanne (EPFL) took a close look at adipose cell subpopulations. They did so by using single-cell RNA sequencing to analyze adipose cells across different adipose niches. Ultimately, they characterized several distinct adipose cell subpopulations, including one that appears to play a role in the accumulation of omental fat, which is associated with the “apple” body shape and a greater risk for metabolic disease.
The scientists, led by Bart Deplancke, PhD, professor at EPFL, reported their findings in Cell Metabolism, in an article titled, “A human omentum-specific mesothelial-like stromal population inhibits adipogenesis through IGFBP2 secretion.”
“[We] provide a comprehensive overview of gene expression profiles of stromal vascular fraction–adherent cells over 30 human donors in four major human depots,” the article’s authors wrote. “We analyzed the main human adipose stem and progenitor cell (hASPC) subpopulations that are common and divergent across depots, as well as their transcriptional and functional characteristics. Furthermore, we established a sorting strategy to isolate, quantify, and characterize different cellular subpopulations … Finally, we identified a new and omentum-specific cell population that inhibits the adipogenic differentiation of hASPCs and hinted at its biomedical relevance by uncovering a significant correlation between inferred insulin-like growth factor binding protein 2 (IGFBP2)-expressing (IGFBP2+) cell abundance and BMI.”
The expansion of omental adipose tissue associated with increased risk for metabolic diseases is not due to the formation of new fat cells, a process known as adipogenesis, but mostly through the enlargement of existing cells, a process called hypertrophy. This can lead to chronic inflammation and insulin resistance.
The limited capacity of omental fat to form new fat cells, despite calorie excess, contrasts with subcutaneous fat and remains poorly understood. However, this aspect of omental fat is a little clearer now that the EPFL team has identified a population of cells in human omental adipose tissue that hinders adipogenesis. This discovery provides a new angle on the limited ability of omental fat to perform adipogenesis and has significant implications for obesity management.
The researchers identified a population of cells present in the omental adipose tissue that may well be the key to explaining its unusual properties. These cells, termed mesothelial cells, generally line certain internal body cavities as a protective layer.
Among these mesothelial cells, some strangely transitioned closer to mesenchymal cells, which can develop into a variety of cell types including adipocytes (fat cells). This dynamic transition between cellular states may be a key mechanism through which these cells exert their influence on the adipogenic potential of the omental adipose tissue.
The study found that the mesenchymal-like properties of these cells are associated with an enhanced ability to modulate their microenvironment, providing a regulatory mechanism for limiting the expansion of adipose tissue. By switching between these two states, the cells may thus be able to influence the overall metabolic behavior of the omental fat depot and its capacity to accumulate fat without triggering metabolic complications.
“Importantly, we also uncovered at least part of the molecular mechanism by which this new omental cell population affects adipogenesis,” said Radiana Ferrero, PhD student at EPFL and one of the study’s lead authors. “Specifically, the cells express high levels of IGFBP2, a protein known to inhibit adipogenesis, and secrete this protein in the cells’ microenvironment. This in turn affects specific receptors on nearby adipose stem and progenitor cells, effectively preventing them from developing into mature fat cells.”
“The findings have deep implications for understanding and potentially managing metabolically unhealthy obesity,” explained Pernille Rainer, PhD, a postdoctoral researcher at EPFL and another lead researcher on the study. “Knowing that omental fat has a built-in mechanism to limit fat cell formation could lead to new treatments that modulate this natural process. Furthermore, the research opens up possibilities for targeted therapies that could modulate the behavior of specific fat depots.”