Collaborating scientists at the Karolinska Institute and at Stockholm University used a technology called in situ sequencing (ISS) to help reveal at the cellular level how lesions in multiple sclerosis (MS) develop. Through their studies and analyses in mice with experimental autoimmune encephalomyelitis (EAE)—a model for MS—and in human tissue, the team spatially mapped MS neuropathology at a single-cell resolution, to unveil cellular architecture and dynamics underlying disease evolution. They suggest that their findings could point to novel targets for multiple sclerosis therapy.

![Castelo Branco Goncalo [Photo: Ulf Sirborn]](https://www.genengnews.com/wp-content/uploads/2024/03/low-res-17-e1711032402116.jpeg)
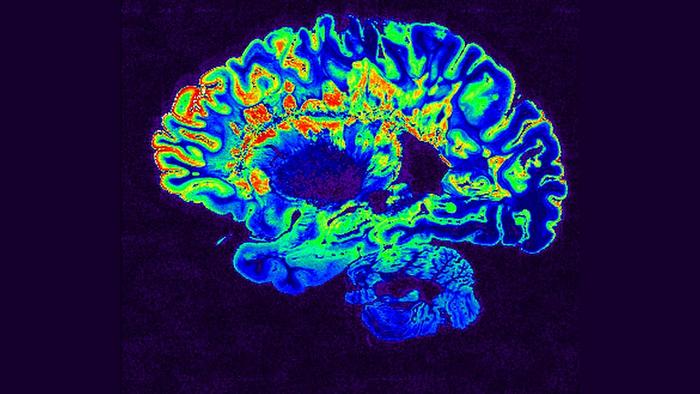
MS is characterized by lesions in the brain and the spinal cord. The authors further explained, “Multiple sclerosis (MS) is a complex disease of unclear, multifactorial etiology and lesion pathology. Lesions, defined by inflammation, gliosis, demyelination, and/or neurodegeneration, affect the white and gray matter (WM and GM) of the central nervous system (CNS).”
![Mats Nilsson [Photo: Olof Lasthein]](https://www.genengnews.com/wp-content/uploads/2024/03/low-res-18-219x300.jpeg)
ISS involves analyzing and identifying cells that are part of a tissue section by reading which genes are active in a particular cell. This single-cell spatial expression profiling reveals both how different cell types are arranged in the tissue—in this case the spinal cord—and how the cells interact with each other. To study how the MS lesions develop, the researchers took samples at different times from the EAE mouse models, and from human MS patients. “The subcellular spatial resolution allowed us to map the dynamics of cell-to-cell interactions and establish the sequence of cellular events during EAE lesion development,” the team wrote. “We correlated our findings with the human MS cytopathology from post-mortem cervical spinal cords …”

In the mice, it was possible to see that the lesions first appeared in the spinal cord and then spread towards the brain. In samples of the spinal cord from four deceased MS patients, 260 genes were simultaneously analyzed and the cellular architecture of the lesions could be determined. The researchers also found new lesions and new sub-structures within the lesions. “… we uncovered spatial preferences of homeostatic and DA-glia within human spinal cord samples, aligning with our observations in mice,” they reported. “We demonstrated that disease-associated (DA)-glia arise independently of lesions and are dynamically induced and resolved over the disease course … Single-cell spatial mapping of human archival MS spinal cords confirmed the differential distribution of homeostatic and DA-glia, enabled deconvolution of active and inactive lesions into sub-compartments, and identified new lesion areas.”
Previously, oligodendrocytes have mainly been seen as victims of immune cell attacks. “The fact that they are active in the outer regions of lesions but also in the entire brain and spinal cord raises the question of whether they dampen the disease or drive it,” Kukanja noted. “… our results indicate that several aspects of MS neuropathology, including certain glial states and their distributions, are common to the mouse EAE and human MS pathologies,” the team continued. “Our study provides insights into the dynamics of MS disease evolution, uncoupling global neuropathology from lesion evolution and uncovering cellular and molecular pathways that may constitute novel targets for MS therapies.”
The two research groups have had an extensive and fruitful collaboration since 2019 and to which they have contributed their respective expertise—from the Karolinska Institute on the cell biology behind MS and from Stockholm University with their pioneering technology in situ sequencing and new methodology for complex image analysis. The scientists next want to use the same methodology to analyze samples from additional MS patients, as the disease is very heterogeneous. Another question they aim to answer is what the lesions look like when patients have received different types of treatments.