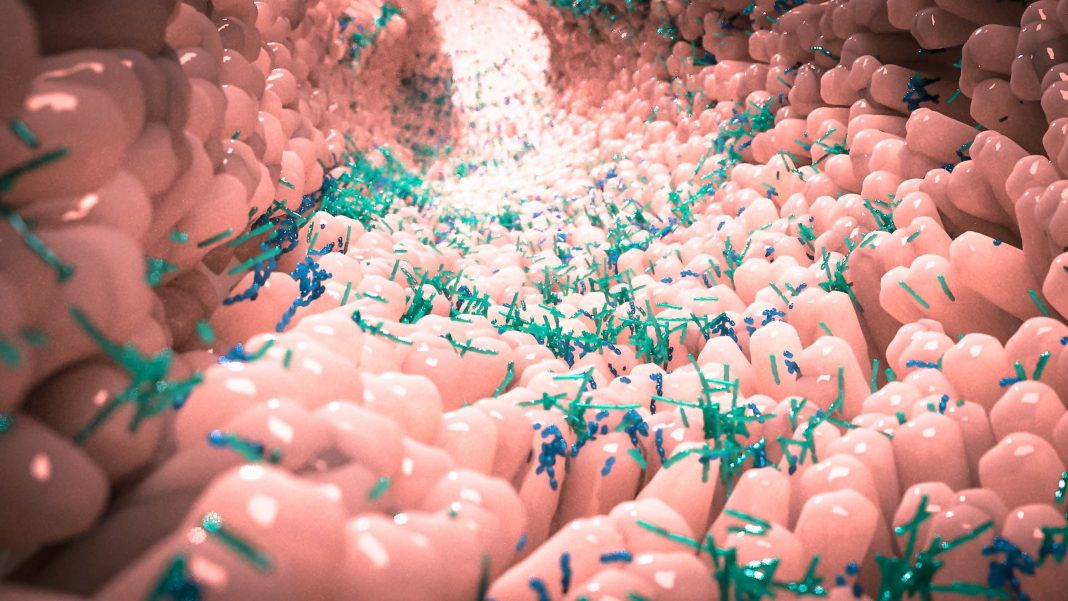
The gut microbiota have a known role in modulating gut immune homeostasis. Largely, through the development and function of host immune cells, including T helper cells expressing interleukin-17A. It has been shown that the bile acid metabolite 3-oxolithocholic acid (3-oxoLCA) inhibits TH17cell differentiation, however, the bacterial source of 3-oxoLCA was previously unknown. Also unclear was the connection between 3-oxoLCA (and other immunomodulatory bile acids) and inflammatory pathologies in humans.
Now, a new study identifies human gut bacteria and corresponding enzymes that convert the secondary bile acid lithocholic acid into 3-oxoLCA as well as the abundant gut metabolite isolithocholic acid (isoLCA). Overall, the authors write, the study suggests that bacterially produced bile acids inhibit TH17 cell function, an activity that may be relevant to the pathophysiology of inflammatory disorders such as inflammatory bowel disease.
This work is published in Nature in the paper, “Human gut bacteria produce ΤΗ17-modulating bile acid metabolites.”
“We carry trillions of bacteria in and on our bodies, and a growing body of research indicates that gut bacteria can affect host immune responses,” said Jun Huh, PhD, associate professor of immunology at Harvard Medical School. “Our findings provide a novel mechanistic insight into how these bacteria work to mediate immune regulation in the gut.”
Bile acids made by the liver have long been known for their critical role in helping to absorb the food we ingest. An initial report mapped out the effects of bile acids on mouse gut immunity, but left some key questions unanswered such as how do bile acids influence gut immune cells to perform their immune-regulatory work, which bacteria and bacterial enzymes produce these bile acids, and do the bile acids play a role in human intestinal inflammation?
Now, this study adds further clarity to the initial observations. The research identifies three bile acid metabolites and corresponding bacterial genes that produce molecules that affect the activity of inflammation-regulating immune cells. More specifically, the team reports that, “Similar to 3-oxoLCA, isoLCA suppressed TH17 cell differentiation by inhibiting retinoic acid receptor-related orphan nuclear receptor-γt, a key TH17-cell-promoting transcription factor.”
The work also demonstrates that the presence and activity of these bacteria and the immune molecules they produce are notably reduced in patients with inflammatory bowel disease (IBD). The authors write, “The levels of both 3-oxoLCA and isoLCA and the 3α-hydroxysteroid dehydrogenase genes that are required for their biosynthesis were significantly reduced in patients with inflammatory bowel disease. Moreover, the levels of these bile acids were inversely correlated with the expression of TH17-cell-associated genes.”
The findings, based on experiments in mice and human stool samples, reveal the identity of three critical microbial players in this cascade and the bacterial genes that regulate bile acid modification. Furthermore, they show that intestinal samples from patients with conditions such as ulcerative colitis or Crohn’s disease have markedly lower levels of both the anti-inflammatory molecules and the bacterial genes responsible for their production. In doing so, they bring scientists a step closer to developing small-molecule treatments and live bacterial therapeutics that regulate intestinal inflammation.
“All three molecules and the bacterial genes that we discovered that produce these molecules are reduced in patients with IBD,” said Sloan Devlin, PhD, assistant professor of biological chemistry and molecular pharmacology at Harvard Medical School. “Restoring the presence of either the compounds or the bacteria that make them offers a possible therapeutic avenue to treat a range of inflammatory diseases marked by these deficiencies and affecting millions of people worldwide.”