As nucleic acid sequencing has become dazzlingly fast, accurate, and affordable, sequencing a whole genome has gone from a trumpeted accomplishment to another day at the office. Now, metagenomic sequencing enables researchers to study an entire collection of genomes from a mixed population of microorganisms simultaneously. This is invaluable for understanding human or animal microbiomes, diagnosing infections, or monitoring emerging pathogens.
Metagenomics seems poised to make the jump from the laboratory bench to the clinic. In 2014, the first case report demonstrated successful use of metagenomics for diagnosis and treatment in a critically ill patient. At the University of California, San Francisco (UCSF), Charles Y. Chiu, MD, PhD, professor of laboratory medicine and medicine/infectious diseases, led a scientific team that detected neuroleptospirosis in a cerebrospinal fluid sample via sequencing, after a conventional infectious disease workup revealed nothing. The patient then received the appropriate antibiotic treatment and recovered.
Since then, multiple metagenomics services have arisen. The UCSF Center for Next-Gen Precision Diagnostics will perform metagenomic sequencing on cerebrospinal fluid or plasma samples, with a 1–2-week turnaround. Karius provides the Karius test, which detects over 1,000 pathogens by sequencing cell-free DNA from plasma, with results typically returned in a day or two. And Arc Bio offers Galileo ONE, a fully integrated in-house workflow, compatible with Illumina sequencers and requiring no prior bioinformatics expertise. Arc Bio claims that Galileo ONE, which can analyze either DNA, RNA, or both, can detect and quantify more than 99% of known human pathogens from a single sample.
Laboratories and hospitals around the world are testing the waters of clinical metagenomics and achieving promising results.
“It’s still an emerging field, but it’s now commonly accepted as being the new frontier for diagnosis of infectious diseases,” says Etienne Ruppé, PhD, professor of medicine at the University of Paris. He cautions, however, that “there are still many hurdles before it can be applied routinely in laboratories.”
Rapid pathogen identification in respiratory infections
The gold standard in diagnostic microbiology is analysis of microorganisms grown in culture from patient samples. A faster alternative that has been gaining acceptance is the use of PCR tests that can identify microbial DNA or RNA. Rapid molecular assays, however, are limited to detecting a predefined subset of pathogens.
Metagenomic sequencing, by contrast, can characterize all the DNA or RNA present in a sample. Although sequencing isn’t quite as fast as PCR testing, it’s much quicker than growing and analyzing a culture.
An opportunity to test metagenomics for diagnosing nosocomial infections in a vulnerable population arose when the COVID-19 pandemic hit. Pathologist Jonathan Edgeworth, PhD, director of the Centre for Clinical Infection and Diagnostics Research (CIDR), Kings’ College London, observed that COVID-19 patients were massing in intensive care units (ICUs), increasing the risk of hospital-acquired infections.
Intubation and other interventions put patients at risk for infections in a couple of ways. A pathogen can hitch a ride from patient to patient on an incompletely sterilized instrument. Other times, a microbe that ordinarily lives harmlessly on the body gets introduced into a new environment, such as the lungs or the bloodstream, and causes a dangerous infection.
Typically, clinicians will start a patient on an antibiotic based on a best-guess diagnosis rather than wait for the analysis to come back. Indiscriminate use of antibiotics can contribute to the development of multidrug-resistant pathogens, however.
“There’s a real absence of comprehensive microbiology information on the day that you’re making the clinical decisions about what to treat with,” Edgeworth says. “When nanopore sequencing came along, we felt that it was potentially something that could provide a lot of what culture provides.”
Nanopore sequencing allows real-time analysis of long DNA fragments, and the long reads enable better species identification. “This is extremely useful for us,” stresses Themoula Charalampous, PhD, a postdoctoral research fellow at CIDR. “We want our workflow to be as rapid as possible. We want to have same-day results.”
Although multiplex PCR assays that test for 20 or more species often suffice, they still leave a degree of uncertainty if the infection isn’t caused by one of the microbes in the test. “When you’re there in the ICU, that’s not good enough,” Edgeworth insists. “The thing about metagenomics is that it sequences everything. It is the equivalent of the culture plate that you’d normally get three days later, but given to you on that day.”
Charalampous and Edgeworth participated in a study that showed nanopore sequencing could detect pathogens with high sensitivity and predict antimicrobial resistance in a real-world clinical ICU setting. The nanopore workflow provided same-day results, and with EPI2ME, an automated data analysis platform offered by Oxford Nanopore Technologies, it eliminated the need for an expert bioinformatician to interpret the results.
Still, it’s a bit too labor intensive for widespread clinical use. “It takes approximately eight hours, and a lot of that is hands-on time,” Charalampous points out. “It requires good molecular biology skills.”

Beware the “kitome”
In the nanopore sequencing study, the researchers intentionally selected patients who clinicians flagged as likely to have an infection. “We didn’t want to put through lots of negative samples,” Edgeworth notes. “It was a proof-of-concept study.”
In routine metagenomic analyses, however, it is often necessary to incorporate negative control samples to account for the microbes commonly found in DNA extraction kits, that is, to account for the so-called kitome. “When we sequence samples that are actually negative, metagenomics sequencing always yields bacterial names,” notes Ruppé. “There are always signatures of DNA. This is what we call the kitome.”
Supposedly sterile labware still carries trace amounts of DNA. Further complicating matters, the kitome can yield different organisms each time. Coping with the kitome isn’t as simple as disregarding a few known contaminants. “This is a very big challenge for us,” Ruppé insists. “The bacteria found in the kitome can also be pathogens.”
For instance, Cutibacterium acnes bacteria are commonly found on the skin, and so they often contribute to the kitome. “In bone and joint infections of the shoulders, it’s also a notorious pathogen,” Ruppé notes. If a possibly infected shoulder sample comes back positive for C. acnes, it would be impossible to differentiate between a true positive and a contaminant.
This is a major issue because of the way metagenomics is typically used. In most cases, conventional microbiology techniques still have the edge in terms of cost, extensive clinical validation, widespread availability, and ability to accurately diagnose most typical infections. Where metagenomics really shines, at least for now, is in solving the most challenging cases, in which conventional methods have yielded no answers.
“Clinical metagenomics has been positioned as a ‘last resort’ diagnosis possibility, when every other method has failed,” Ruppé maintains. “But if everything else has failed, then there is a good chance that the sample is actually negative, so you have to deal with contaminants.”
Early detection of life-threatening infections
As metagenomics technology becomes more automated and affordable, broader application of the technology becomes more feasible. For example, metagenomics could be used to advantage earlier in patient care. “This is the question now in clinical metagenomics,” Ruppé says. “Should we use it only as a last resort test? What would be the benefit of using it at earlier stages?”
Evidence is growing that clinical metagenomics should be considered alongside existing methods, not just after all else fails. According to Natacha Couto, PhD, associate researcher at the University of Bath, there are many reports in the literature suggesting that metagenomics is more sensitive than culture, as well as many reports suggesting that it does not. Couto emphasizes, however, that many studies indicate that metagenomics does complement culture.
“There are plenty of examples where … metagenomics identified potential microbes that were not identified by culture alone,” Couto notes. “Just like PCR became complementary to culture once it was introduced, this will happen with metagenomics as well.”
Using metagenomics sooner could help stop infections before they become symptomatic, saving money, shortening hospital stays, and reducing patient stress. David Haslam, MD, pediatrician and director of the Microbial Genomics and Metagenomics Laboratory at Cincinnati Children’s Hospital Medical Center, sees a role for metagenomics in monitoring vulnerable patients after antibiotic treatment.
“If your microbiome becomes abnormal in a certain way, we’re trying to use that as a predictor for future infection,” Haslam says. He cites a case in which a patient’s normal, diverse microbiome became disrupted after a course of antibiotics, and a particular Escherichia coli strain came to dominate.
When the patient developed a severe bloodstream infection, sequencing revealed that the invading bacteria were of the very same strain that had taken over the gut microbiome. Monitoring the gut microbiome could provide advance warning of such an infection. The Karius test, Haslam adds, can detect bacterial DNA in the bloodstream before any outward signs of infection have emerged.
“[Monitoring the microbiome is] very exciting because it might point toward interventions that you can do before a patient becomes ill,” Haslam explains. “But from a diagnostic standpoint, it gets very confusing. Are we picking up organisms in the gut that are not causing infection? Those things can probably be understood better with more experience, but I think right now there is that problem.”
Another problem is that metagenomics can pick up nucleic acid signatures of organisms that are already dead, Couto points out. Consider a case where a patient has an infection and begins treatment, but the symptoms continue. Even if the treatment is working, she says, metagenomic sequencing could pick up lingering DNA from the dead microbes. Couto maintains that it’s “up to the clinician to combine all the data that is available, including data about the symptoms and the laboratory methods that have been used, to define whether something is an infection or not.”
Metagenomics give us a better way to detect antibiotic resistance. “PCR tests provide rapid, accurate information about antibiotic resistance genes, but those tests look at only a few antibiotic resistance genes,” Haslam explains. “In theory, metagenomics could look at every antibiotic resistance gene.”
However, widening that net requires a certain caution, he points out. Whereas the PCR tests can focus on genes that are strongly correlated with antibiotic resistance, metagenomics will catch genes that are less certain. For instance, a metagenomics application would need to distinguish between members of gene families that share sequence similarity but confer different degrees of resistance.
“That’s mostly a bioinformatics challenge and a computational challenge,” Haslam remarks. “I think there’s a future there, and it’s probably several years off, but I think machine learning is going to be the answer to sorting out those gray zones.”
Long-read sequencing to distinguish between close cousins
Another such gray zone is distinguishing between similar bacterial species where small genomic changes can mean the difference between a harmless commensal and a dangerous pathogen. It can be difficult to tease apart closely related species using metagenomics techniques, because all the genomes are mixed together in the sample.
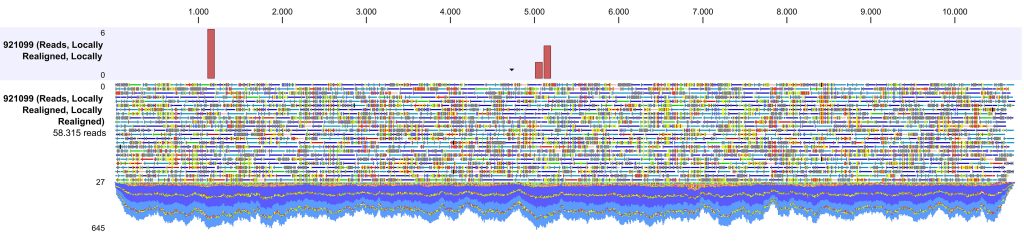
According to a recent study (Bickhart et al. Nat. Biotechnol. 2022; DOI: 10.1038/s41587-021-01130-z), researchers from the U.S. Department of Agriculture and the University of California, San Diego, overcame this problem with deep sequencing using PacBio’s HiFi read technology, which generates long reads with greater than 99.9% accuracy. When the researchers used the technology to sequence the sheep fecal metagenome, they were able to assemble truly complete bacterial genomes without getting stuck on highly repetitive segments. They binned the contigs using high-throughput chromosome conformational capture (Hi-C), and then used an algorithm called MAGPhase to resolve closely related haplotypes.
Ultimately, the study identified 428 genomes with more than 90% completeness, 44 of them in single circular contigs. These findings indicate that a complete metagenomics approach could be successful in assessments of other metagenomes, including human metagenomes.
One of the study’s leaders, Pavel A. Pevzner, PhD, a professor of computer science at the University of California, San Diego, suggests that metagenomic techniques could help us cope with bacterial outbreaks like the 2011 E. coli outbreak in Germany. “It was not that easy to sequence the pathogenic E. coli strain that caused the outbreak,” he recalls. “I’m confident that in the future if there are bacterial outbreaks, people will definitely be using this complete metagenomics approach to define pathogenic species. The cost is negligible compared to the billions of dollars that can be lost in outbreaks.”
“Metagenomics is moving to a new era,” Pevzner declares. “[Our study] is simply a signal that this new era has already come.”

