Scientists from the Icahn School of Medicine at Mount Sinai (MSSM) have published a study that describes the biological mechanism used by a family of proteins called histone deacetylases to activate immune system cells linked to inflammatory diseases. Their work is detailed in a new paper published in Proceedings of the National Academy of Sciences (PNAS) titled, “Class IIa HDAC4 and HDAC7 cooperatively regulate gene transcription in Th17 cell differentiation.”
Eighteen HDACs have been identified in mammals that act as epigenetic regulators and post-transcriptional modifiers. As the PNAS paper’s title indicates, the researchers studied class IIa HDACs, which have more tissue-specific functions unlike some of the other four HDAC classes, such as class I HDACs, which act more broadly.
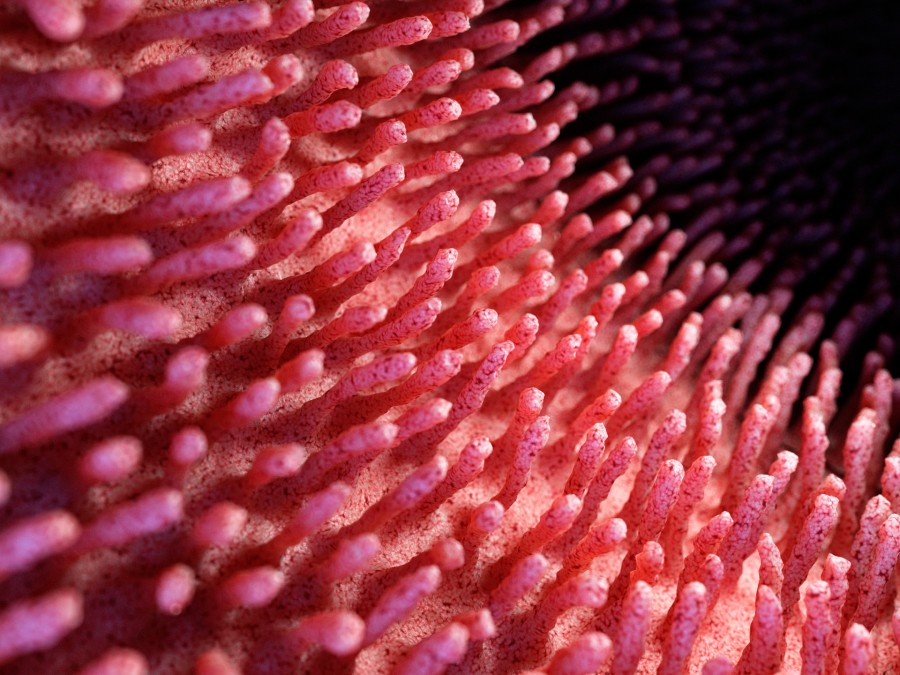
Specifically, they looked at two class II HDACs—HDAC4 and HDAC7—which regulate the development and differentiation of T-helper 17 cells from CD4+ T cells. These cells produce interleukin-17 (IL-17), an inflammatory cytokine associated with disorders like IBD, multiple sclerosis, and rheumatoid arthritis. The MSSM research identified a mechanism that HDAC4 and HDAC7 use to “orchestrate both gene transcriptional activation and repression to steer the process of Th17 cell differentiation,” noted Ka Lung Cheung, PhD, an assistant professor of pharmacological sciences at MSSM and lead author on the study.
The correlation between excessive Th17 cell activity and human disease lead scientists to believe that pharmacological or genetic interventions that target HDAC4/7 can successfully mitigate Th17 cell-mediated inflammation. To date, “our understanding of the specific function of class II HDACs in different cell types has been limited, impeding development of therapies targeting this promising drug target family,” said senior author Ming-Ming Zhou, PhD, a professor of physiology and biophysics and chair of MSSM’s department of pharmacological sciences. These results provide “essential knowledge to explore their therapeutic potential for safer and more effective disease treatments.”
HDAC inhibitors have previously been used to treat cancer and shown promise for treating other disorders including neurodegenerative, cardiovascular, and inflammatory diseases. To date, the FDA has approved four HDAC inhibitors for cancer including Vorinostat and Romidepsin, both of which are used to treat cutaneous T-cell lymphoma.
The MSSM researchers believe that their findings could lead to new kinds of HDAC inhibitors for treating some types of inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease. In fact, as part of the study, the researchers identified a potential class IIa HDAC inhibitor called TMP269. Using a mouse model of inflammatory bowel disease (IBD), specifically ulcerative colitis, they demonstrated that this molecule successfully influenced Th17 differentiation.
But there may be other opportunities to develop inhibitors for class II HDACs as therapies for diseases other than beyond IBD. In fact, “we believe our findings pave the way for extensive research into advanced therapies targeting severe inflammation in various other pathologies within the human body,” Zhou said.