Institute for Systems Biology researchers have found that the gut microbiome is partly responsible for the differences in circulating blood metabolites across people. The team studied variability in plasma metabolites in more than 1,500 individuals for whom paired genomic and metabolomics data were available. The results indicated that nearly two-thirds of the more than 900 blood metabolites were largely associated with either genetics or with the gut microbiome, and 70% of those associations were driven solely by the microbiome.
The findings, the investigators suggested, will help direct future development of targeted interventions designed to alter the composition of the human blood metabolome. “A deeper understanding of the determinants of the blood metabolome will provide us with a window into how these circulating metabolite levels can be engineered and optimized for health,” said Andrew Magis, PhD, who is co-corresponding author of the team’s published paper in Nature Metabolism. “Understanding which circulating small molecules fall predominantly under host versus microbiome control will help guide interventions designed to prevent and/or treat a range of diseases.”
Added Sean Gibbons, PhD, an ISB faculty member, “We know that person-to-person variation in the blood metabolome—the small molecules found in the bloodstream that can interact with all the systems of our body—can tell us a lot about health and disease status. Figuring out what governs this variation is a necessary step that gets us closer to precision approaches to healthcare. Gibbons is co-corresponding author of the researchers’ paper, which is titled, “Genome–microbiome interplay provides insight into the determinants of the human blood metabolome.”
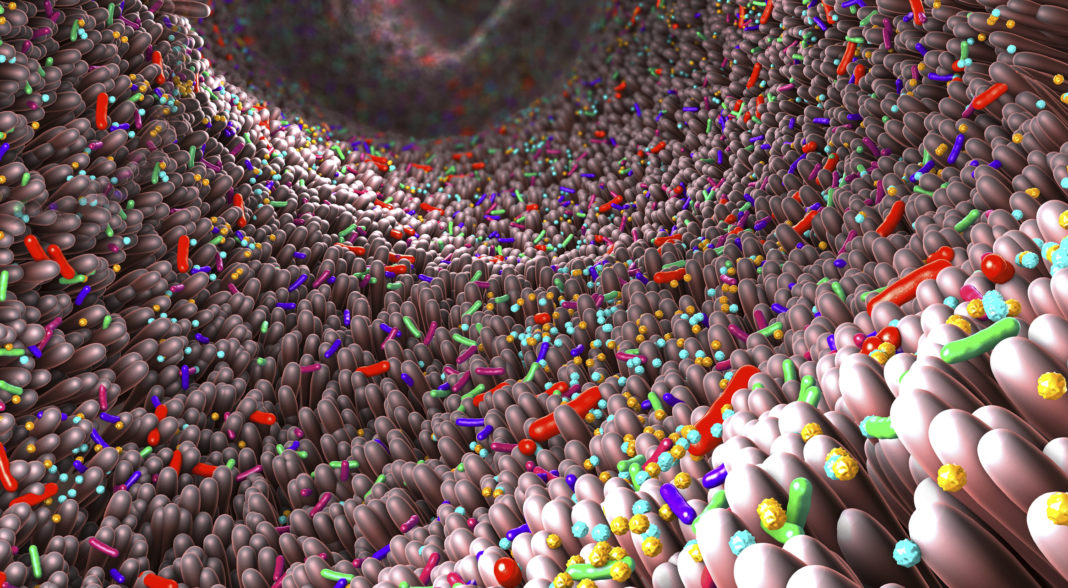
The human blood metabolome is shaped by a combination of intrinsic and extrinsic factors, and represents the primary resource pool for human metabolism, the authors noted. The composition of the plasma metabolite pool is affected by diet, lifestyle, and the gut microbiome, as well as by genetics. Genetic variants are known to alter the human blood metabolome in several disease-relevant contexts, and recent studies have also identified the human gut microbiome as a major determinant of blood metabolite variability. But while variation in the blood metabolome is intimately related to human health, the investigators continued, “few details are known about the interplay between genetics and the microbiome in explaining this variation on a metabolite-by-metabolite level.”
For their study, the ISB research team, headed by co-lead authors Christian Diener, PhD, senior research scientist, and Chengzhen Dai, PhD, the researchers analyzed de-identified metabolomic, genomic, and microbiome data from consenting patients in a consumer scientific wellness program. They examined 930 blood metabolites that were present in more than 1,500 individuals. After controlling for potential covariables, the investigators found that 64% of the detected metabolites were significantly associated with either host genetics or the gut microbiome.“Notably, 69% of these associations were driven solely by the microbiome, with 15% driven solely by genetics and 16% were under hybrid genetic-microbiome control,” said Diener.
The scientists found that the blood metabolite variation explained by the microbiome was largely independent of the variation explained by the genome, even for hybrid metabolites that were significantly associated with both genetics and microbes. Additionally, certain metabolite-microbe associations were only significant in individuals with specific genetic backgrounds, indicating a nuanced interplay between the microbiome and host genetics in shaping the blood metabolome.
“Overall, our analyses show that the plasma metabolome is influenced by the interplay between genetic and microbial factors, where the abundances of individual microbially derived metabolites absorbed in the gut are often affected additively by variation in both host genetics and gut ecology,” the team commented.
These new findings offer up interesting insights. The high number of microbiome-specific metabolites suggests that much of our blood metabolome could be modified through dietary, probiotic, and other lifestyle interventions. But also, metabolites that are under stricter genetic control may not be responsive to lifestyle modification, making them targets for pharmacological interventions that directly target host pathways.
“ … many microbe–metabolite associations are dependent upon host genetic background,” the authors wrote. “These hybrid genome–microbiome–metabolite models provide unique insights into the forces underlying variation in the human blood metabolome and can suggest possible therapeutic strategies … we suggest that disease-relevant blood metabolites strongly associated with the microbiome may be modifiable through dietary, probiotic, prebiotic, or lifestyle interventions whereas metabolites under strong genetic control may require pharmacological interventions that target host metabolic pathways.”