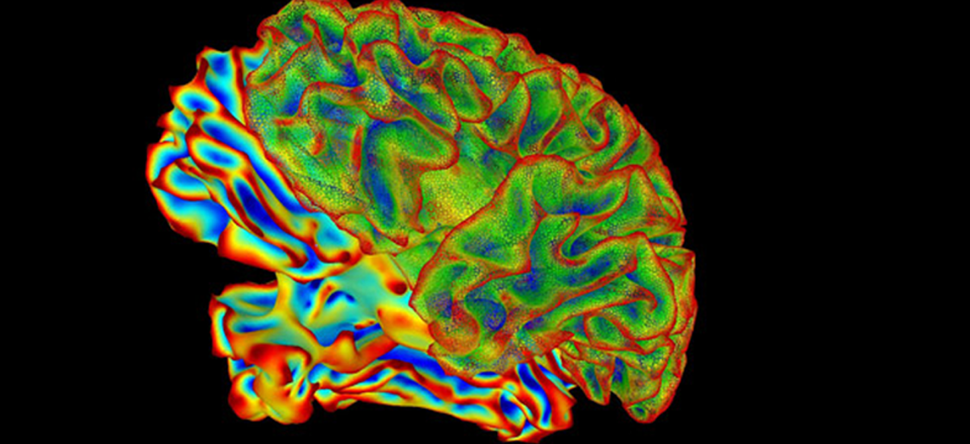
Researchers at Baylor College of Medicine, and the University of California, San Francisco (UCSF), have used both genetic and pharmacologic approaches to reverse learning and memory deficits associated with Down syndrome (DS), in a standard mouse model of the disorder. The researchers’ studies were focused on the role of the integrated stress response (ISR), a conserved mechanism that helps to maintain protein homeostasis, or proteostasis, by regulating protein synthesis. They found that some of the intellectual impairments associated with Down syndrome were linked to ISR activation and altered protein production in the hippocampus region of the brain—which is central to learning and long-term memory formation—in both the mouse model and in postmortem samples from Down syndrome patients. Modulating ISR in the mouse model significantly improved cognitive function in the animals.
Although the cognitive features of DS have generally been thought of as irreversible, the findings indicate that it may be possible to develop drugs that improve cognitive function in human DS. “In the last 10 years, we and others have shown the ISR is a molecular switch for normal long-term memory formation. In this study, we found that the switch is off in Down syndrome,” said Mauro Costa-Mattioli, PhD, a professor of neuroscience at Baylor College of Medicine. “More importantly, turning the switch back on in these mice reverses their memory deficits. These very encouraging results suggest that tuning the ISR may emerge as a promising avenue to alleviate a wide range of cognitive disorders with a disruption in protein homeostasis.”
The researchers report their findings in Science, in a paper titled, “Activation of the ISR mediates the behavioral and neurophysiological abnormalities in Down syndrome.”
Intellectual disability affects about 2–3% of the population, the authors stated. Down syndrome results from an extra copy of human chromosome 21, and the disorder is the most common genetic cause of intellectual disability.
To identify proteostasis-related problems that might contribute to DS, the researchers turned to the ts65Dn mouse, an animal model that recapitulates the genetic, behavioral, and cognitive features of human Down syndrome. Using polysome profiling, a technique that allows scientists to take a detailed snapshot of the cell’s protein factories in action, Walter, Costa-Mattioli, and colleagues found that up to 39% less protein was being produced in the hippocampus of the DS mice. This prompted them to ask why extra copies of genes could lead to a decline in protein production.
The researchers’ experiments indicated that hippocampal cells in DS mice had activated the ISR. This biological circuit effectively detects when something’s not right—the presence of an extra chromosome, in the case of DS—and engages a response that activates machinery to tamp down protein production. “The cell is constantly monitoring its own health,” Walter commented. “When something goes wrong, the cell responds by making less protein, which is usually a sound response to cellular stress. But you need protein synthesis for higher cognitive functions, so when protein synthesis is reduced, you get a pathology of memory formation.”
The scientists subsequently found that the ISR was also activated in postmortem samples of brain tissue from human patients with DS. Of particular interest, they were able to obtain a tissue sample from a Down syndrome patient in whom some cells had a third copy of chromosome 21, while other cells were genetically normal. They found that in these samples, the ISR was only active in the cells with the extra chromosome. Taken together, the findings strongly suggested that the ISR is involved in, and perhaps responsible for, certain DS symptoms. “Thus, activation of the ISR in the brains of Ts65Dn mice and human individuals with DS provides a common molecular signature of the condition,” the investigators wrote.
Motivated by the findings so far, Costa-Mattioli and his colleagues investigated whether the activation of the ISR mediated the long-term memory deficits in Down syndrome. To answer this question, they used different genetic and pharmacological manipulations to correct the ISR in the Down syndrome mouse model.
The ISR can be activated by four different enzymes; the scientists found that only one of them, PKR, was involved in activating the ISR in hippocampal cells in DS. They tested three different approaches to reducing ISR activity. Either deleting the PKR gene, or using a drug that suppresses PKR activity, or employing a safe, well-studied drug called ISRIB, which activates protein-manufacturing machinery that competes directly with the ISR’s efforts to shut off protein production. Each strategy resulted in a marked improvement in cognition in the animals, demonstrated by two different memory and learning tests. Blocking PKR activity effectively prevented ISR activation and reversed the decline in protein production that had been observed in the brains of DS mice. Encouragingly, the researchers found that blocking ISR also significantly improved cognitive function in the animals. “Given the heterogeneity of the genetic perturbations in DS, it seems unlikely that aberrant levels of a single protein are the sole cause of the long-term memory deficits associated with DS,” the researchers noted. “Instead of repairing the expression of individual genes, we correct the overall translational program controlled by the ISR.”
“Down syndrome mice exhibit problems with long-term memory,” commented first author Ping Jun Zhu, PhD, assistant professor of neuroscience and senior investigator in the Costa-Mattioli group. “In one set of experiments, we trained Down syndrome and control mice in a new task. Down syndrome mice did not learn the task as well as control mice. However, when we genetically or pharmacologically inhibited the ISR, the animals were able to learn almost as well as control mice.”
The researchers also measured the strength of the synaptic connections in the Down syndrome mice and found that the connections were not as strong as those in control mice. But inhibiting the ISR in Down syndrome mice was able to reverse the deficits in synaptic function. After blocking ISR activity the brains of DS mice transmitted fewer inhibitory signals that can make it harder for the brain to learn and form new long-term memories. At the cellular level, synaptic plasticity—the ability to form neural connections—is believed to be a central mechanism that could explain how memories are formed. The new findings support the researchers’ hypothesis that activation of the ISR network mediates the memory deficits associated with Down syndrome. “Thus, the ISR plays a crucial role in DS, which suggests that tuning of the ISR may provide a promising therapeutic intervention,” the authors concluded.
Although results from the reported studies are promising, Walter acknowledged that far more research will be needed. Even so, the work represents an important first step towards finding potential therapies for Down syndrome, a condition that has generally been considered untreatable. “We started with a situation that looked hopeless,” Walter said. “Nobody thought anything could be done. But we may have struck gold.” Costa-Mattioli added: “In the current study, we investigated the role protein homeostasis networks play in Down syndrome. A decline in protein homeostasis networks is strongly linked to several neurological conditions, from aging to neurodegenerative disorders, but little was known about its role in Down syndrome.”
DS is characterized by a high incidence of early onset AD [Alzheimer’s disease], and activation of the ISR has been implicated in a variety of neurodegenerative disorders, including AD, traumatic brain injury, prion disease, and myelination disorders, the team stated. “Thus, genetic or pharmacological modulation of the ISR may emerge as a promising avenue to alleviate a wide range of cognitive disorders resulting from a disruption in protein homeostasis.”
“In the last 10 years, we and others have shown the ISR is a molecular switch for normal long-term memory formation,” Costa-Mattioli said. “In this study, we found that the switch is off in Down syndrome. More importantly, turning the switch back on in these mice reverses their memory deficits. These very encouraging results suggest that tuning the ISR may emerge as a promising avenue to alleviate a wide range of cognitive disorders with a disruption in protein homeostasis.”