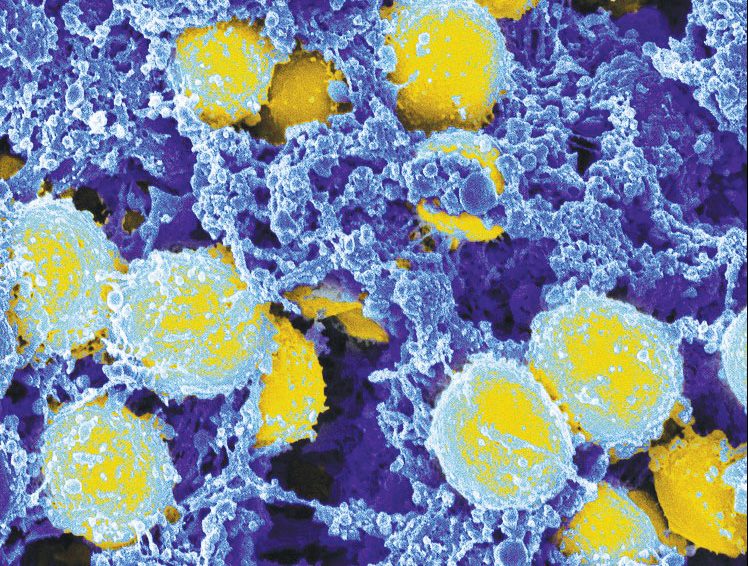
Staphylococcus aureus is a gram-positive bacteria that causes a wide variety of clinical diseases. Infections caused by this pathogen are common both in community-acquired and hospital-acquired settings. Infections can be life-threatening if the bacteria enter the bloodstream, causing sepsis. Now, researchers led by the Peter Doherty Institute for Infection and Immunity analyzed the genetic profiles of more than 1,300 staph strains and uncovered what makes the bacterium so dangerous when it enters the blood.
The findings are published in Cell Reports in an article titled, “A statistical genomics framework to trace bacterial genomic predictors of clinical outcomes in Staphylococcus aureus bacteremia.”
“Outcomes of severe bacterial infections are determined by the interplay between host, pathogen, and treatments,” the researchers wrote. “While human genomics has provided insights into host factors impacting Staphylococcus aureus infections, comparatively little is known about S. aureus genotypes and disease severity. Building on the hypothesis that bacterial pathoadaptation is a key outcome driver, we developed a genome-wide association study (GWAS) framework to identify adaptive mutations associated with treatment failure and mortality in S. aureus bacteremia (1,358 episodes). Our research highlights the potential of vancomycin-selected mutations and vancomycin minimum inhibitory concentration (MIC) as key explanatory variables to predict infection severity.”
By combining this data with patient and antibiotic information, the researchers found that, while patient factors are critical in determining mortality risks, specific genes are linked to antibiotic resistance, along with the bacteria’s ability to linger in the blood, evading antibiotics and the immune system.
“To the best of our knowledge, this is one of the first times that the method we used, called a genome-wide association study (GWAS), has been applied to delve into the role of bacterial genomes, host factors, and antibiotics on the course of staphylococcal sepsis,” said Stefano Giulieri, MD, PhD, a clinician-researcher at the Doherty Institute and first author of the paper.
“In GWAS, scientists scan the genome of a big collection of bacteria to look for tiny changes (mutations) that show up more often in strains with a certain characteristic, such as antibiotic resistance. Mutations with a strong statistical link are precious clues to figuring out how bacteria acquire attributes that are important for patient outcomes.
“Our study uncovered a deeper understanding of the intricate genetic dynamics underlying severe Golden staph infections. It highlights the potential of combining bacterial whole-genome sequencing, clinical data, and sophisticated statistical genomics to discover clinically relevant bacterial factors that influence infection outcomes.”
“By revealing the genes responsible for antibiotic resistance in Golden staph, our GWAS is pointing the scientific community to clearer targets for the development of effective solutions to treat Golden staph bloodstream infections,” said University of Melbourne professor Ben Howden, director of the Microbiological Diagnostic Unit (MDU) Public Health Laboratory at the Doherty Institute and co-senior author of the paper.
“This knowledge has the potential to shape and enhance our ability to tackle these persistent infections. As bacterial genomes become increasingly available in the clinical routine, we inch closer to customized therapeutic strategies, where treatments will be tailored to the unique genetic makeup of the infecting strain, rather than treating everyone in the same way.”