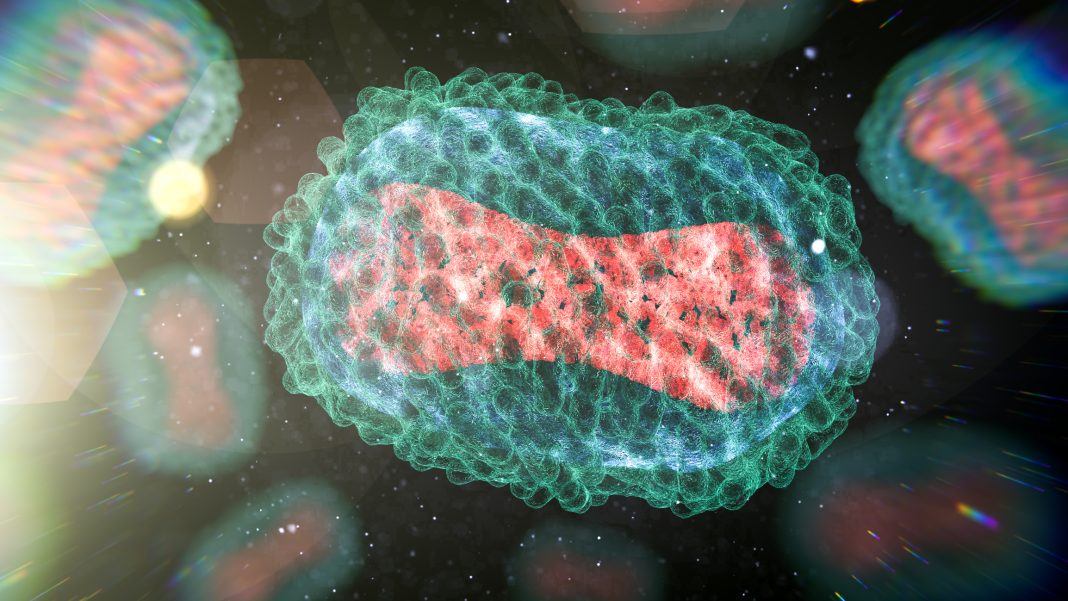
A recent Monkeypox virus (MPXV) outbreak (consisting of 92,000 Mpox cases in 110 nonendemic countries since 2022) has put a spotlight on the need for a highly efficient vaccine.
Now, a new vaccine candidate from Moderna, mRNA-1769, has been shown to more effectively limit symptoms and disease duration in primates that were infected with a lethal strain of the mpox virus when compared to a currently licensed MPXV vaccine.
The study was published in Cell in the paper, “Comparison of protection against Mpox following mRNA-1769 or MVA vaccination in NHPs”.
The primary vaccine being used in the current outbreak is the JYNNEOS vaccine; Modified Vaccinia Ankara (MVA) (known internationally as Imvamune or Imvanex and manufactured by Bavarian Nordic) is a live virus that does not replicate efficiently in humans. The MVA vaccine has been shown to reduce transmission in at-risk populations but fails to completely protect. There have also been lags in manufacturing and distribution of MVA during the outbreak.
Now, mRNA-1769, an mRNA-LNP vaccine expressing MPXV surface proteins, was tested in a lethal MPXV primate model. Similar to MVA, mRNA-1769 conferred protection against challenge, but with improved mitigation of symptoms and disease duration.
“This study is the first in a nonhuman primate model where we compare an investigational mRNA mpox vaccine directly to the current standard of care,” said Alec Freyn, PhD, a principal scientist at Moderna. “When we put those vaccines head-to-head in primates, we saw improved responses from the mRNA vaccine in terms of not just protection from survival but also fewer lesions, shorter duration of disease, and less viral shedding in the blood and respiratory tract.”
To directly compare the investigational mRNA vaccine to MVA vaccines, the researchers vaccinated six macaques with each vaccine and then exposed them to a lethal strain of mpox virus eight weeks after their initial vaccine dose. They also exposed a control group of six unvaccinated animals to the virus. Following infection, the researchers monitored the animals’ health for four weeks and collected blood samples to examine their immune response.
All 12 vaccinated animals survived the challenge, regardless of which vaccine was used, whereas five of six unvaccinated control animals succumbed to the disease. Though both vaccines reduced disease severity compared to the control group, mRNA-vaccinated animals lost less weight and had fewer lesions than MVA-vaccinated animals—on average, animals in the control group had a maximum of 1,448 lesions, MVA-immunized animals had a maximum of 607 lesions, and mRNA-immunized animals had a maximum of 54 lesions.
The mRNA vaccine also shortened disease duration (the number of days for which the animals showed lesions) by more than 10 days compared to the MVA vaccine and resulted in lower viral loads in both blood and throat swabs, suggesting that it might also be more effective at reducing transmission.
“With the mRNA technology, we’re able to produce a vaccine that gives quite potent responses with a very tolerable safety profile,” said Jay Hooper, PhD, chief, molecular virology branch at United States Army Medical Research Institute for Infectious Diseases (USAMRIID). “We’ve been trying to get a vaccine that will prevent spread like ACAM2000 but without the safety issues. This is showing that mRNA technology might be able to fill that niche.”
When the researchers compared the immune response triggered by the mRNA and MVA vaccines, they found that the mRNA vaccine resulted in higher numbers of antibodies, as well as antibodies with more diverse immune functions. More specifically, the authors noted that antibody profiling revealed “a collaborative role between neutralizing and Fc-functional extracellular virion (EV)-specific antibodies in viral restriction, and ospinophagocytic and cytotoxic antibody functions in protection against lesions. mRNA-1769 enhanced viral control and disease attenuation compared to MVA, highlighting the potential for mRNA vaccines to mitigate future pandemic threats.”
The mRNA vaccine also showed potential to induce cross-immunity to other orthopoxviruses, whereas the MVA vaccine results in smaller immune responses that are not as strongly neutralizing for more remotely related orthopoxviruses.
“We tested serum from the monkeys immunized with this vaccine against basically every orthopoxvirus we could get our hands on,” says Freyn. “It neutralized not only mpox but also vaccinia, cowpox, rabbitpox, camelpox, and ectromelia virus. We believe that this vaccine may protect from other orthopoxvirus threats that may emerge in the future.”
Moderna’s mRNA-1769 vaccine is currently being assessed in a Phase I/II clinical trial (NCT05995275) to determine the safety, tolerability, and immune response of a range of doses of mRNA-1769.