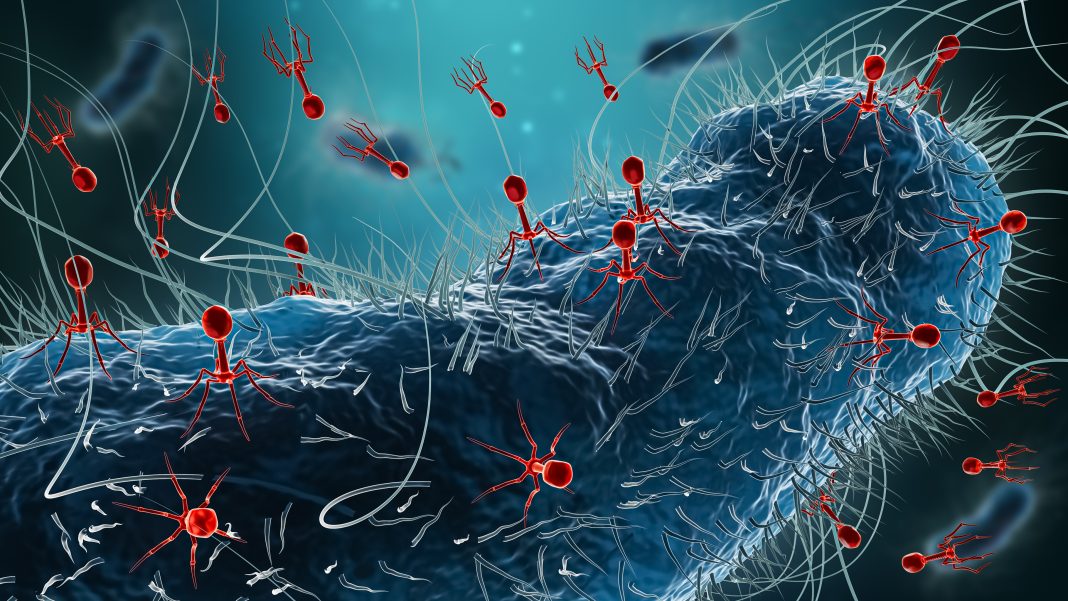
In an effort to illustrate that genomic surveillance can build the foundation for scaleable precision phage therapy, an international collaboration analyzed the genomes of over 15,000 cases of Acinetobacter baumannii. In doing so, they traced the global existence and spread of this critically antibiotic-resistant bacteria commonly found within hospitals, building the first “superbug map.” They noted that this work will aid in the development of lifesaving bacteriophage therapies and could advance the phage therapy market by streamlining clinical trials and boosting global collaborations.
The team, led by scientists at the HUN-REN Biological Research Centre in Szeged, Hungary, identified the dominant bacterial strains from around the world, showing that the superbug species spread relatively slowly and remained dominant for approximately six years in a given country. The work highlights the timeframe that hospitals may have to apply pre-emptively prepared bacteriophages for treatment as “off-the-shelf” region-specific phage therapies that could address up to 80% of local infections.
This work is published in Cell, in the paper, “Genomics surveillance as a scalable framework for precision phage therapy against antibiotic-resistant pathogens.”
“Currently many bacterial infections cannot be effectively treated and phages offer a promising alternative or complementary therapy to combat the rising number of hospital-acquired antibiotic-resistant infections,” said Balint Kintses, PhD, group leader at the Laboratory of Translational Microbiology at HUN-REN Biological Research Centre. “This is where our map offers a groundbreaking solution for phage therapy. By analyzing how superbugs spread and dominate in hospitals, we can now prepare region-specific phage treatments in advance.”
One of the key challenges of phage therapy is that each patient requires a specific phage to treat their infection. Therefore, phages are currently used to treat mostly chronic infections where there is time to find the matching phage to target the infection-causing bacteria, a process that is expensive and time-consuming.
However, the greatest need for phage therapy is in acute, antibiotic-resistant bacterial infections where patients die within days if a treatment cannot be found. The “superbug map” enables the production of pre-emptive phage treatments based on the Acinetobacter baumannii strains most likely to cause infections in each region.
To build the map, a large-scale analysis of over 15,000 genome sequences of Acinetobacter baumannii from public databases from 85 countries across five continents was used to assess the geographical distribution of these strains. Additionally, the team collected samples from 44 hospitals in five Eastern European countries from COVID-19 ventilated patients with secondary, antibiotic-resistant bacterial infections.
Using phylogeographical methods, the dominant bacterial strains in different regions were identified and their distribution tracked. These data were combined with high-throughput phage typing to understand which bacteriophages are effective against specific strains, enabling the development of targeted therapies.
The hope is that this work will be able to help healthcare providers significantly improve the management of infections that develop quickly and don’t respond to antibiotics.
“To reach this strategic goal, the superbug map will help clinicians identify patients for phage therapy clinical trials, accelerating the validation and approval process for these treatments,” added Kintses. “Researchers using the mapping framework will be able to access global data and share insights, contributing to a worldwide effort to combat antibiotic resistance through precision medicine approaches and bring phage treatments to the patients who need them most.”