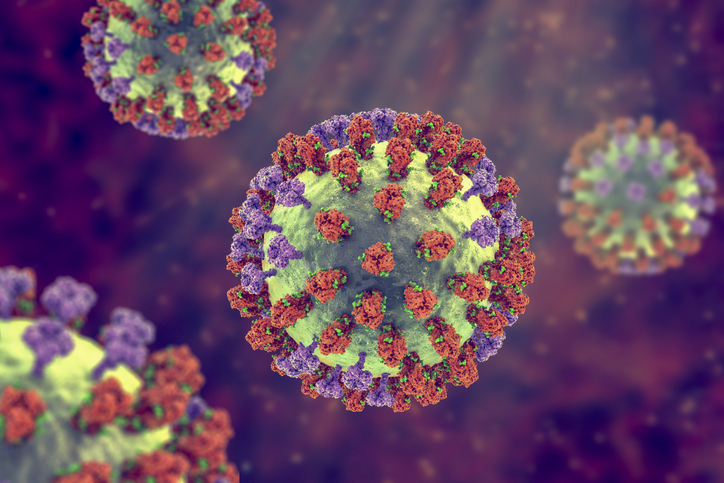
Just over a month ago, in Texas, a person tested positive for the highly contagious influenza H5N1 strain, otherwise known as highly pathogenic avian influenza (HPAI) or “bird flu” or “avian flu.” (The highly pathogenic terminology refers to the virus when infecting birds, not humans.)
HPAI can be transmitted by wild birds to domestic poultry and other bird and animal species. It is somewhat uncommon to see avian flu infections in humans, making the recent case of the human infection in Texas notable. The patient, who had exposure to dairy cows, reported eye redness (common with conjunctivitis) as their only symptom.
This one infection does not change the H5N1 bird flu human health risk assessment for the U.S. general public, which the Centers for Disease Control and Prevention (CDC) still considers to be low. However, the CDC is closely monitoring the situation and using its flu surveillance systems to monitor H5N1 activity in people. The last case of a human infection with H5N1 was in 2022, in Colorado, which was linked to exposure to poultry.
The presence of H5N1 in dairy cows was first reported in Texas and Kansas by the U.S. Department of Agriculture (USDA) on March 25, 2024. As of April 26, the number of cases of H5N1 flu that had been detected in wild birds was 9,296. There were 90,827,876 cases in poultry and 34 dairy herds have been infected. Nine states have reported infected cattle: Idaho, Colorado, Michigan, Texas, New Mexico, South Dakota, Kansas, North Carolina, and Ohio.
What about the milk supply?
The FDA posted an update on April 25 with information regarding the analysis of influenza in milk. These data were from a commercial milk sampling study from across the country (297 samples of retail dairy products from 38 states) in coordination with USDA. The initial results showed that about 1 in 5 of the retail samples tested were qPCR-positive for HPAI viral fragments (with a greater proportion of positive results coming from milk in areas with infected herds).
The agency emphasized that “positive results do not necessarily represent actual virus that may be a risk to consumers.” In order to further clarify the risk to consumers, two questions need to be answered: 1) are intact viruses present in the milk and 2) if so, are they infectious?
The FDA is conducting further testing, including egg inoculation tests which can determine the presence of infectious virus. On April 26, the FDA published an update with additional results. They noted that “preliminary results of egg inoculation tests on quantitative polymerase chain reaction (qPCR)-positive retail milk samples show that pasteurization is effective in inactivating HPAI.”
To clarify, the testing did not detect any live, infectious virus. In addition, samples of retail powdered infant formula, and powdered milk products marketed as toddler formula, were all negative using qPCR testing.
The FDA will continue testing. Samples that test positive with PCR will undergo egg inoculation tests. But because the early testing indicates no sign of infectious virus in retail milk, the FDA concluded that there is no reason to think that the commercial milk supply is unsafe. They also stressed that these results do not apply to unpasteurized milk, which carry a higher risk.
The agency added that data from the CDC’s epidemiology work show that cases of flu—in general—are not increasing and that there have been no reported cases of H5N1 beyond the case in Texas. The efforts to gather information, they emphasized, are ongoing and they will share their results from the egg inoculation tests as soon as possible.
One thing is for certain; everyone is watching this story closely. Right now, the risk remains low. There is one case of H5N1 in a person who worked closely with cattle. But the risk will increase if one of two things happens: 1) an increase in the number of cases of humans infected from cattle or 2) a case of human-to-human transmission. Either of these, and in particular the latter, will increase the cause for concern.