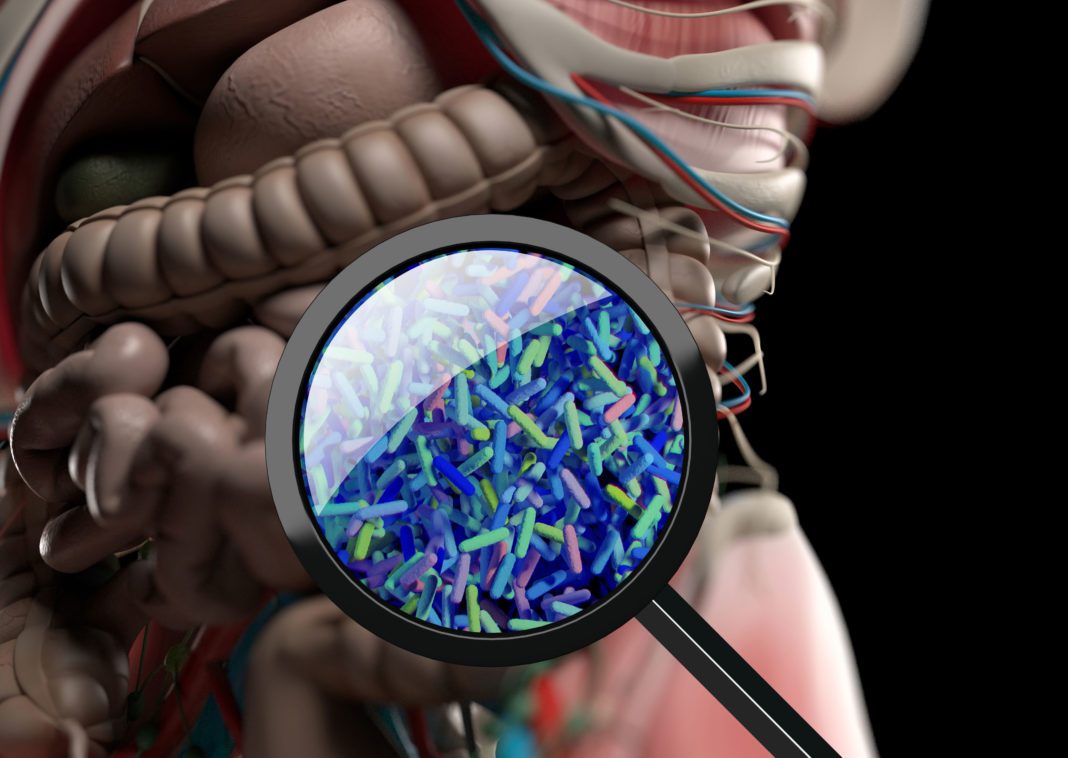
Inflammatory bowel disease (IBD) is a broad term that describes conditions characterized by chronic inflammation of the gastrointestinal tract. The two most common inflammatory bowel diseases are ulcerative colitis and Crohn’s disease. Several types of medications may be used to treat IBD such as aminosalicylates, corticosteroids (such as prednisone), immunomodulators, and “biologics.” Now, researchers from Brigham and Women’s Hospital report they have developed an engineered yeast that can induce multiple effects for treating IBD. Their preclinical results could potentially affect the lives of thousands of patients with IBD.
Their findings are published in Nature Medicine in a paper titled, “Self-tunable engineered yeast probiotics for the treatment of inflammatory bowel disease.”
“IBD is a complex chronic inflammatory disorder of the gastrointestinal tract,” wrote the researchers. “Extracellular adenosine triphosphate (eATP) produced by the commensal microbiota and host cells activates purinergic signaling, promoting intestinal inflammation and pathology. Based on the role of eATP in intestinal inflammation, we developed yeast-based engineered probiotics that express a human P2Y2 purinergic receptor with up to a 1,000-fold increase in eATP sensitivity.”
“We’ve taken yeast—the very yeast that’s used to make beer—and we’ve given it the ability to sense inflammation and secrete an anti-inflammatory molecule,” explained Francisco Quintana, PhD, an investigator in the Ann Romney Center for Neurologic Diseases at Brigham and a corresponding author of the study. “We call this new platform ‘Y-bots’ (yeast robots) and see the potential here for developing therapeutics that can treat diseases of the gut tissue and more.”
The Quintana lab previously discovered the connection between the gut and diseases that affect the brain.
In the current study, the researchers developed their probiotic using Saccharomyces cerevisiae, a species of yeast used in winemaking, baking, and brewing. Using CRISPR/Cas9, they introduced genetic elements that could sense inflammation and respond to it by secreting an enzyme that can degrade a key molecule involved in inflammation.
The engineered yeast suppressed intestinal inflammation in mice, reducing and restoring a balanced gut microbiome.
“By combining directed evolution and synthetic gene circuits, we developed a unique self-modulatory platform for the treatment of IBD and potentially other inflammation-driven pathologies,” the researchers wrote.
The researchers plan to further refine and test the engineered yeast to see if they can speed up tissue repair. They also plan to investigate the use of engineered probiotics for treating a common side effect of cancer immunotherapy, colitis.
“We want to use the tools of synthetic biology to engineer what can be found in nature,” concluded Quintana. “By engineering probiotics, our goal is to create more personalized, localized, and highly controlled medications for treating diseases of the gut and beyond.”