Some researchers are thinking outside the box to try to combat the growing antibiotic resistance crisis. One of the innovations has been the development of “living medicines” which use one living bacterium to kill another. In a new study, researchers developed a modified (non-pathogenic) version of Mycoplasma pneumoniae that attacks Pseudomonas aeruginosa—which is resistant to many types of antibiotics and is a common source of infections in hospitals. The modified M. pneumoniae was used in combination with low doses of antibiotics that would otherwise not work on their own.
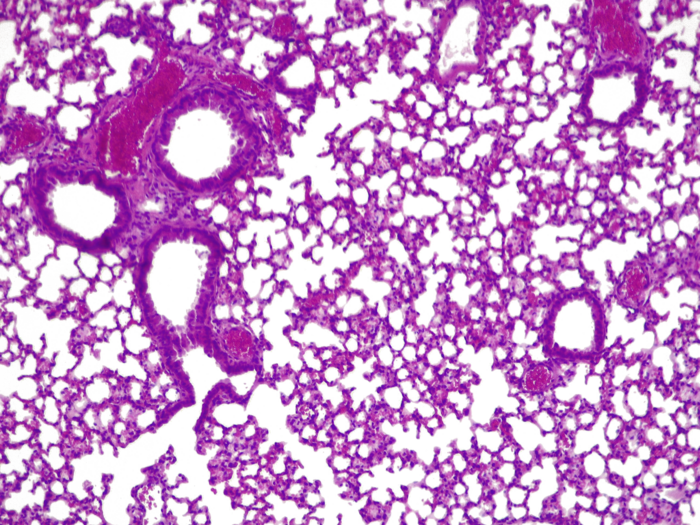
The M. pneumoniae treatment significantly reduced lung infections in mice and doubled mouse survival rate compared to no treatment. Administering a single, high dose of the treatment showed no signs of toxicity in the lungs. And, once the treatment had finished its course, the immune system cleared the modified bacteria in a period of four days.
This research is published in Nature Biotechnology in the paper, “Engineered live bacteria suppress Pseudomonas aeruginosa infection in mouse lung and dissolve endotracheal-tube biofilms.”
P. aeruginosa infections are difficult to treat, in part, because the bacteria forms biofilms which have an increased resistance to antibiotics.
One particularly challenging infection occurs when biofilms grow on the surface of endotracheal tubes used by critically-ill patients who require mechanical ventilators to breathe. This causes ventilator-associated pneumonia (VAP), a condition that affects one in four (9–27%) patients who require intubation. The incidence exceeds 50% for patients intubated because of severe COVID-19. VAP can extend the duration in the intensive care unit for up to thirteen days and kills up to one in eight patients (9–13%).
In this study, M. pneumoniae was engineered to dissolve biofilms by equipping it with the ability to produce various molecules including pyocins—toxins naturally produced by bacteria to kill or inhibit Pseudomonas. To test its efficacy, they collected P. aeruginosa biofilms from the endotracheal tubes of patients in intensive care units. They found the treatment penetrated the barrier and successfully dissolved the biofilms.
“We have developed a battering ram that lays siege to antibiotic-resistant bacteria. The treatment punches holes in their cell walls, providing crucial entry points for antibiotics to invade and clear infections at their source. We believe this is a promising new strategy to address the leading cause of mortality in hospitals,” said María Lluch, PhD, staff scientist in the lab of Luis Serrano Pubul, PhD, at the Centre for Genomic Regulation (CRG) at the Catalan Institution for Research and Advanced Studies (ICREA) in Barcelona, Spain, and CSO at Pulmobiotics.
M. pneumoniae is one of the smallest known bacterial species. With just 684 genes and no cell wall, the relative simplicity of M. pneumoniae makes it ideal for manipulation. One of the advantages of using M. pneumoniae to treat respiratory diseases is that it is naturally adapted to lung tissue.
“The bacterium can be modified with a variety of different payloads—whether these are cytokines, nanobodies, or defensins. The aim is to diversify the modified bacterium’s arsenal and unlock its full potential in treating a variety of complex diseases,” said Serrano.
In addition to designing the “living medicine,” Serrano’s research team is also designing new proteins that can be delivered by M. pneumoniae to target inflammation caused by P. aeruginosa infections. The inflammatory response is orchestrated by the release cytokines. One type of cytokine—IL-10—has well-known anti-inflammatory properties and is of growing therapeutic interest.
Research published by Serrano’s lab in the journal Molecular Systems Biology designed new versions of IL-10 optimized to treat inflammation. The cytokines were designed to be created more efficiently and to have higher affinity, meaning fewer cytokines are needed to have the same effect.
They then engineered strains of M. pneumoniae that expressed the new cytokines and tested their efficacy in the lungs of mice with acute P. aeruginosa infections. The engineered versions of IL-10 were significantly more effective at reducing inflammation compared to the wild-type IL-10 cytokine.
“Live biotherapeutics such as M. pneumoniae provide ideal vehicles to help overcome the traditional limitations of cytokines and unlock their huge potential in treating a variety of human diseases,” noted Ariadna Montero Blay, a PhD student in the Serrano lab. “Engineering cytokines as therapeutic molecules was critical to tackle inflammation. Other lung diseases such as asthma or pulmonary fibrosis could also stand to benefit from this approach.”