It was only a matter of time. Once genome editing tools established themselves in biomedical science—advancing enterprises such as the development of cell lines, the dissection of disease mechanisms, and the identification of drug targets—they were bound to have their potential tested in clinical science. Indeed, genome editing–based gene therapies began to be studied in clinical trials in 2020. Since then, the number of these therapies in clinical trials has kept growing.
In a recent preprint (Eshka et al. A systematic review of gene editing clinical trials. medRxiv. November 25, 2022), the number of gene editing clinical trials was put at 76. Of these trials, 30 were related to genetically engineered T-cell therapies for cancer, 19 were related to virus infections, and 26 were related to monogenic diseases (of which 21 were related to monogenic blood diseases).
The preprint also indicated that in most of the studies, gene editing had been accomplished with CRISPR-Cas technology. Nonetheless, a significant portion of the studies involved the use of other technologies, such as zinc finger nuclease (ZFN) technology and transcription activator-like effector nuclease (TALEN) technology.
The counts tallied toward the end of 2022 are probably due for an update already. But rather than indulge in that exercise, this article will highlight a few representative gene editing clinical trials—representative in the sense that they demonstrate the range of gene editing technologies. Specifically, CRISPR, ZFN, and TALEN technologies are mentioned, as well as a meganuclease technology. The selection of clinical trials also suggests how a range of conditions is being addressed. For example, clinical trials are cited that involve transthyretin amyloidosis, sickle-cell disease, and lysosomal storage disorders.
CRISPR-based clinical trials for transthyretin amyloidosis
NTLA-2001, an investigational therapy based on CRISPR-Cas9 genome editing, was developed as a result of a partnership between Intellia Therapeutics and Regeneron Pharmaceuticals to treat transthyretin amyloidosis, a proteinopathy in which transthyretin forms amyloid fiber aggregates in tissues. “Intellia and Regeneron’s transthyretin amyloidosis therapy candidate is the first example of CRISPR being used in vivo for a therapeutic application,” asserts David Gutstein, MD, vice president and global program head at Regeneron Pharmaceuticals.
Physiologically, transthyretin exists in the plasma as a circulating tetramer. In patients harboring transthyretin mutations, or rarely with aging, the tetramer can break down into individual monomers, which are taken up into tissues (mainly the heart and peripheral nerves), undergo misfolding, agglomerate, and disrupt tissue function. “As a result, a person may experience cardiomyopathy, polyneuropathy, or both,” Gutstein says.
Therapies that became available in recent years for transthyretin amyloidosis include stabilizers of the protein tetramer structure and silencers that knock down gene expression by either small interfering RNA or antisense oligonucleotides. “The ability to slow disease progression by knocking down transthyretin levels with RNA silencers provided the clinical validation for our therapeutic strategy,” Gutstein notes.

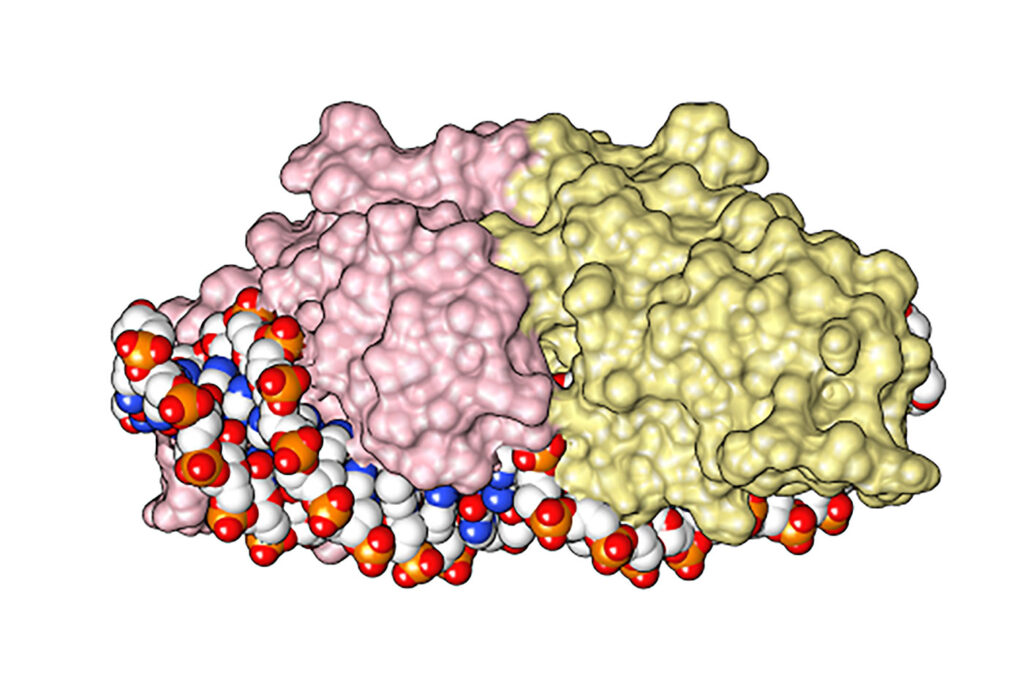
NTLA-2001 is based on a guide RNA, which specifically recognizes the transthyretin gene, and an mRNA molecule that encodes the Cas9 nuclease, both packaged into lipid nanoparticles that are administered intravenously. The nanoparticles are taken up by hepatocytes in the liver, where the guide RNA and the mRNA are released into the cytoplasm. Cas9 mRNA is translated into the Cas9 nuclease and forms a nucleoprotein complex with the guide RNA, which traffics to the nucleus and inactivates the transthyretin gene.
Interim data from an ongoing Phase I study evaluating NTLA-2001 as a treatment for transthyretin amyloidosis show benefits for participants in both the cardiomyopathy and the polyneuropathy arms, including a marked and sustained decrease in serum transthyretin levels that approached maximal effect 28 days after treatment. “Single doses of NTLA-2001 were administered to patients with transthyretin amyloidosis with polyneuropathy or cardiomyopathy,” Gutstein says. “The team found a dose-dependent effect in knocking down transthyretin protein in the bloodstream, which consistently exceeded 90% knockdown at the highest doses tested.”
NTLA-2001 was generally well tolerated, and the protein knockdown persisted for at least 6–12 months of follow-up. The one-time administration of the product may potentially enable a durable, lifetime solution to the disease.
Prior to the clinical trials, NTLA-2001 was studied in cell-based assays, biochemical experiments, and computer programs to predict potential off-target sites. “The team invested extensive effort into establishing the specificity of our agent before initiating clinical trials,” Gutstein relates. “We have a high degree of confidence that our CRISPR therapeutic will affect only the target gene of interest.” These studies showed that at a margin significantly above clinically relevant concentrations, the treatment did not affect any targets besides the transthyretin gene.
Another challenge in developing NTLA-2001 involved translating the dose from animal models into human patients. “Because this was the first time a systemically delivered in vivo CRISPR therapeutic was moving forward into the clinic, we dedicated a lot of attention to patient safety, and specifically into how to predict the dose in human patients based on animal data, and that understanding will inform future CRISPR-based platforms as well,” Gutstein says.
The partnership between Regeneron and Intellia catalyzed the development of an additional program, which uses Intellia’s proprietary CRISPR platform to insert a functional gene into the genome. “That is one level of complexity above performing a simple knockout,” Gutstein notes. “For us, it represents the next step in treating patients with genetic diseases.” The first investigational product being developed as part of this collaboration aims to treat hemophilia B, a clotting disorder in which a genetic mutation leads to a deficiency of factor IX, a vitamin K–dependent plasma protein.
Making fetal hemoglobin in sickle-cell disease
“Drug discovery is the ultimate team sport, in the sense that there isn’t any single thing that has to go right, but thousands of different things need to be done carefully and meticulously to bring a medicine to patients,” says David Altshuler, MD, PhD, executive vice president, global research, and chief scientific officer, Vertex Pharmaceuticals.
A major collaborative effort between Vertex and CRISPR Therapeutics focuses on developing a treatment for sickle-cell disease and b-thalassemia. “We have known the cause of sickle-cell disease since 1949, but nobody has cured it, and this is not because we didn’t know what to do, but because we didn’t know how to do it,” Altshuler explains. Sickle-cell disease results from a point mutation in the b-globin gene that causes hemoglobin to polymerize and become rigid, making the red blood cells adopt a sickle shape and leading to blood vessel obstruction and tissue damage. Patients experience intense pain, during events known as vaso-occlusive crisis and present anemia, hemolysis, and inflammation, which ultimately lead to progressive organ damage and premature death. b-thalassemia is also a genetic disease characterized by inadequate hemoglobin production, which requires blood transfusions to improve the oxygen carrying capacity.
Major considerations in the choice for sickle-cell disease, as one of the areas of focus in the Vertex/CRISPR collaboration, included the great unmet need around this medical condition, the detailed knowledge about its pathogenesis, the severity of the disease, the large number of individuals affected worldwide, and the recent emergence of CRISPR as a technology. “CRISPR was developed about 10 years ago in the laboratory, and now we have filed for approval for the first medicine—a much faster pace than has happened with any previous technology,” Altshuler emphasizes.
The joint Vertex/CRISPR program led to the development of exagamglogene autotemcel (exa-cel), in which a patient’s own hematopoietic stem cells are edited ex vivo using CRISPR-Cas9 to produce high levels of fetal hemoglobin. “After completing regulatory filing in the United Kingdom and the European Union in 2022, in early April 2023 we announced completion of the rolling biologics license application to the FDA,” Altshuler says. This was the first regulatory filing for a CRISPR-based therapy in the United States.
Any gene editing therapy opens two types of safety considerations in terms of potential off-target effects. The first consideration involves the possibility of affecting cell types other than the cell type intended. This concern can be circumvented with exa-cell, which takes an ex vivo approach. The second consideration involves inadvertently editing genomic locations that are different from the intended target. “We have carefully conducted extensive safety studies,” Altshuler notes. “We were unable to detect any off-target genomic effects with exa-cel.”
Developing better enzymes for CRISPR-Cas approaches
“Our approach employs a novel, proprietary CRISPR enzyme called AsCas12a,” says Baisong Mei, MD, PhD, chief medical officer, Editas Medicine. The AsCas12a enzyme has high editing efficiency and specificity, and it is used in EDIT-301, an experimental cell therapy that edits the promoter region of the gamma globin genes 1 and 2 in patient-derived CD34+ hematopoietic stem and progenitor cells. “This mimics the natural mechanism of hereditary persistence of fetal hemoglobin, where a person with sickle-cell disease co-inheriting fetal hemoglobin can have minimal or no symptoms,” Mei explains. Preclinical and initial clinical data show that EDIT-301 leads to robust fetal hemoglobin expression and healthy erythropoiesis.
Two clinical programs that use EDIT-301 are the RUBY trial for the treatment of severe sickle-cell disease and the EDITHAL trial for the treatment of transfusion-dependent b-thalassemia. “In December 2022, we shared initial clinical data from the RUBY trial. Specifically, we shared that a patient who had five months of follow-up at the time of data disclosure showed clinically significant improvements across all hematological parameters and no vaso-occlusive events since treatment with EDIT-301, suggesting clinical proof of concept for EDIT-301,” Mei details. Editas anticipates sharing more clinical data from the RUBY trial in mid-2023, as well as initial clinical data from EDITHAL by late 2023.
Editas is also pursuing in vivo gene editing in hematopoietic stem cells and other cell types for additional diseases. “I believe that in the future we will see several regulatory approvals around the world for the treatment of several devastating diseases that were previously untreatable,” Mei predicts. “This will change the lives of people with serious diseases around the world.”
Clinical trials for lysosomal storage diseases
“Our Phase I/II STAAR study expansion phase is ongoing,” says Jason Fontenot, PhD, chief scientific officer at Sangamo Therapeutics. “We are actively progressing toward a potential Phase III trial, with a start date anticipated by the end of 2023.”
The global, multicenter STAAR trial uses ST-920, an investigational gene therapy product based on a recombinant adenoviral vector that encodes the cDNA for a-galactosidase A. ST-920 was developed by Sangamo for the treatment of Fabry disease, a life-threatening lysosomal storage disorder. Fabry disease is an X-linked inherited metabolic genetic condition caused by mutations in the enzyme a-galactosidase A, which breaks down globotriaosylceramide. As a result of the enzymatic deficiency, large amounts of intracellular globotriaosylceramide build up in the affected patients, leading to multiorgan damage.
Sangamo uses its proprietary ZFN technology to generate therapeutic products. “We have a full spectrum of tools,” Fontenot asserts. “They are smaller, can access the DNA easier, are unconstrained by guiding sequences, and can be packaged better.” He adds that Sangamo’s platform can be used to pursue clinical programs across the spectrum of genomic medicine “from in vivo genome engineering to ex vivo cell and gene therapy.”
Current efforts at Sangamo are focusing on extending the genetically engineered adenoviral capsid platform to deliver genomic medicine into the brain. “This work,” Fontenot says, “has the potential to reshape the way we treat various neurological disorders.”
A talent for TALENs
“Of eight ongoing clinical trials in which TALEN technology is used to generate CAR T-cell products, we fully own four,” says Philippe Duchateau, PhD, chief scientific officer of Cellectis. He adds that two Cellectis partners, Servier Laboratories and Allogene Therapeutics, own the other four.
The TALEN technology is based on highly specific DNA-binding proteins known as transcription activator-like effectors, which have an array of amino acid repeats that can be designed to recognize specific DNA sequences and are fused to the DNA-cleaving domain of the FokI nuclease to allow targeted and highly specific genomic modifications.
Cellectis uses TALEN technology to create allogeneic CAR T-cell products as opposed to autologous products. (An autologous product can be used only in the individual patient that the T cells were derived from.) “The autologous approach is not really a product but rather a process that is applied to a patient’s cells,” Duchateau explains. “In our case, we are creating a biopharmaceutical product.”
The in-house proprietary GMP manufacturing process at Cellectis provides independence and control over product development, improves the opportunity to meet patient needs, and allows scalability and batch-to-batch reproducibility. “It took us some time to do that,” Duchateau says. “But we reached the point where we can now manufacture high-quality products with superior reproducibility.”
One of Cellectis’s wholly owned, allogeneic, off-the-shelf, gene edited T-cell product candidates, UCART22, targets CD22, a multifunctional transmembrane glycoprotein that regulates B-cell survival and signal transduction and is expressed in over 90% of the patients with B-cell acute lymphoblastic leukemia. A Phase I dose-escalation study of intravenous UCART22 in patients with relapsed and refractory B-cell acute lymphoblastic leukemia was initiated in late 2019, and its primary completion date is anticipated to be in 2023. Preliminary results showed encouraging antileukemic activity without unexpected or significant toxicity. In late 2022, Cellectis dosed its first patient in the United States with relapsed or refractory B-cell acute lymphoblastic leukemia with in-house prepared UCART22 and reported no dose-limiting toxicities after a 28-day observation period.
Another product in the Cellectis licensed partners pipeline, ALLO-501A, is an allogeneic CAR T-cell product candidate. It is currently being jointly developed by Servier and Allogene for large B-cell lymphoma. A Phase I, open-label study conducted at eight centers across France, the United Kingdom, the United States, and Japan enrolled adult participants with CD19-positive large B-cell lymphoma and evaluated its antileukemic activity and safety profile.
In August 2022, Cellectis initiated a Phase I/IIa trial with UCART20x22, a dual CAR T-cell product targeting CD20 and CD22 for relapsed and refractory non-Hodgkin’s lymphoma. UCART20x22 was Cellectis’s first dual allogeneic CAR T-cell product candidate to enter clinical development. “Going from liquid tumors to solid tumors (which is still challenging today) and the development of combination therapies will be important future developments in the field,” Duchateau says.
Homing in on cancer
Precision BioSciences is a clinical-stage biotechnology company dedicated to improving life with its novel and proprietary ARCUS genome editing platform. ARCUS is based on a naturally occurring genome editing enzyme, I-CreI, that evolved in the algae Chlamydomonas reinhardtii to make highly specific cuts and DNA insertions in cellular DNA. I-CreI is a member of a larger class of enzymes called homing endonucleases or meganucleases.
The company has multiple allogeneic CAR T-cell immunotherapies in early-stage clinical trials. For example, azercabtagene zapreleucel (azer-cel; PBCAR0191) is an investigational anti-CD19 allogeneic CAR T-cell candidate being evaluated in a Phase I/IIa clinical trial of adult subjects with relapsed or refractory non-Hodgkin’s lymphoma. And PBCAR19B is a next-generation, anti-CD19 immune-evading stealth cell candidate being evaluated in a Phase I study of adult subjects with relapsed/refractory non-Hodgkin’s lymphoma.

