The “hygiene hypothesis” suggests that increased exposure to microorganisms can benefit our health. However, in our modern, relatively sterile world children can be denied this everyday contact with potentially health-boosting bacteria and other microorganisms—call them “old friends”—and studies suggest this can impact on the immune system and even mental health. A team of scientists at the University of Colorado (UC), Boulder, has now identified an anti-inflammatory fat in the soil bacterium Mycobacterium vaccae, which might explain how the organism can dampen stress-related disorders, and could also feasibly help scientists to develop a microbe-based “stress vaccine.”
“We think there is a special sauce driving the protective effects in this bacterium, and this fat is one of the main ingredients in that special sauce,” said integrative physiology professor Christopher Lowry, PhD, who is senior author of the team’s published paper in Psychopharmacology. “This is just one strain of one species of one type of bacterium that is found in the soil but there are millions of other strains in soils. We are just beginning to see the tip of the iceberg in terms of identifying the mechanisms through which they have evolved to keep us healthy. It should inspire awe in all of us.”
Lowry and colleagues reported their findings in a paper titled, “Identification and characterization of a novel anti-inflammatory lipid isolated from Mycobacterium vaccae, a soil-derived bacterium with immunoregulatory and stress resilience properties.”
British scientist David Strachan proposed the “hygiene hypothesis” in 1989, which mooted that a lack of exposure to microorganisms in childhood has led to impaired immune systems and higher rates of allergies and asthma. A more refined version of the hypothesis suggests that it is lack of exposure to beneficial soil and environmental microbes that impacts on our immune systems and even mental health.
“The idea is that as humans have moved away from farms and an agricultural or hunter-gatherer existence into cities, we have lost contact with organisms that served to regulate our immune system and suppress inappropriate inflammation,” said Lowry, “That has put us at higher risk for inflammatory disease and stress-related psychiatric disorders.” The prevalence of anxiety disorders, for example, is now more than 10% in Euro/Anglo cultures, the authors wrote.
Research also suggests that increased inflammation can be a risk factor for trauma- and stress-related disorders such as post-traumatic stress disorder (PTSD). Individuals with PTSD are at an increased risk of developing autoimmune disorders, “suggesting that impaired immunoregulation or inappropriate inflammation may confer risk for development of both autoimmune conditions and PTSD.”
This connection between inflammation, immune system function, and stress response is particular interesting given evidence to indicate that some microorganisms to which humans have been exposed during evolution can actually drive anti-inflammatory and immunoregulatory mechanisms that prevent the body from mounting inappropriate immune responses. “Throughout human evolution, the interactions between these ancestral microorganisms, which we have collectively referred to as ‘old friends,’ and the innate immune system promoted immunoregulation,” the authors stated. “In their absence, the host may develop inappropriate immune responses to allergens, self-antigens, or gut microbiota.
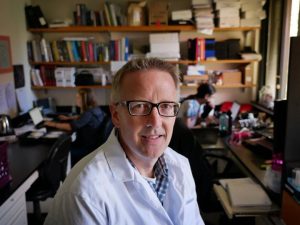
Lowry and colleagues have published multiple studies linking exposure to healthy bacteria and mental health. One such soil bacterium M. vaccae has been found to exhibit immunoregulatory and stress-protective effects in mouse models. Work by Lowry has previously shown that mice pretreated with a heat-killed preparation of M. vaccae were protected from allergic pulmonary inflammation, and that immunizing mice with M. vaccae prior to a stressful event could prevent a “PTSD-like” syndrome, fending off stress-induced colitis and making the animals act less anxious when stressed again later.
The UC Boulder researchers have now identified and synthesized a free fatty acid, 10(Z)-hexadecenoic acid, which is produced by M. vaccae. Studies involving next-generation sequencing demonstrated that the lipid directly interacted with activated immune system macrophage cells, binding to the peroxisome proliferator-activated receptor (PPAR) and inhibiting inflammatory pathways. “It seems that these bacteria we co-evolved with have a trick up their sleeve,” said Lowry. “When they get taken up by immune cells, they release these lipids that bind to this receptor and shut off the inflammatory cascade.”
A series of further studies demonstrated that the lipid acted to upregulate genes linked with peroxisome proliferator-activated receptor (PPAR) signaling, and inhibited proinflammatory signaling by activated macrophages ex vivo. “The effects of 10(Z)-hexadecenoic acid to inhibit proinflammatory signaling of activated macrophages ex vivo were prevented by PPARα antagonists and absent in PPARα-deficient mice,” the authors wrote.
They suggest that their collective findings could help guide the development of new therapeutic approaches. “The identification of specific microbially derived molecules with anti-inflammatory or immunoregulatory properties may provide novel therapeutic avenues for the treatment of diseases of immunodysregulation or trauma- and stressor-related disorders where exaggerated inflammation is thought to be a risk factor.”
The discoveries could feasibly also help scientists move towards developing a “stress vaccine” from M. vaccae, which could be given to personnel such as first responders, or soldiers in high-stress situations, to help protect against the psychological damage of stress. “This is a huge step forward for us because it identifies an active component of the bacteria and the receptor for this active component in the host,” Lowry said.


