Sponsored content brought to you by
Chimeric antigen receptor (CAR) T-cell therapy continues to show great promise with certain subsets of B-cell leukemia or lymphoma. The unique CARs are artificially modified fusion proteins that consist of extracellular antigen recognition domains fused to intracellular co-stimulatory and activation signaling domains. Recent advancements have led to improvements in potency against specific cancer cells and persistence in the immunosuppressive tumor microenvironment, but many challenges remain with toxicity and efficacy of CAR T-cell therapies. A recent study found that 57% of CAR T-cell therapy patients relapse within one year of treatment.1
Leading the Way
ProMab Biotechnologies takes a multidisciplinary scientific approach to develop and commercialize recombinant proteins, antibodies, and engineered cell lines using high-throughput technologies.
Committed to improving human health, ProMab Biotechnologies focuses on the field of immunotherapy, including CAR T-cell, CAR NK-cell, and gamma delta T-cell technologies. Their scientific team has developed >1,000 CAR constructs with different structures, promoters, and signaling domains. Propelled by a strong dedication to this field, ProMab has become the first global CAR T-cell CRO.
Overcoming Patient Relapse

Current CAR T-cell treatments available for multiple myeloma, a cancer affecting plasma cells in the bone marrow, have been shown to extend patient survival. However, patient relapse is common due to downregulation of targets such as B-cell maturation antigen (BCMA), leading to lack of CAR T-cell proliferation.2 “In such cases, combination therapy with bispecific CAR T cells can be very useful. If the BCMA antigen is downregulated, targeting an additional antigen such as CS1, an overexpressed cell surface receptor, is a promising strategy for multiple myeloma cases,” says Vita Golubovskaya, PhD, Director of Research and Development, ProMab.
To overcome the challenge of patient relapse due to BCMA downregulation, the scientists at ProMab discovered a novel CS1 antibody specifically recognizing the CS1 antigen with high activity in CAR format, and developed bispecific CS1-BCMA-CAR T cells to better treat patients with multiple myeloma.3 The bispecific CAR T cells they developed have been shown to effectively block multiple myeloma tumor growth in vivo and provide a basis for future clinical trials. They have also applied the same strategy to address the loss of the CD19 antigen for lymphoma by developing bispecific CD19-CD37 CAR T cells.4
Additionally, their use of bispecific and multispecific CAR T cells for treating multiple myeloma can be extended to solid tumors, which currently has limited efficacy. An ongoing clinical trial at Changsha Hospital in China treated ten patients with several doses of ProMab’s BCMA-CAR T cells and 3 patients with ProMab’s CD37-CD19 CAR T cells. To date, the treatments have shown a good safety profile.
Adopting Key Technologies to Support a Robust CAR Screening Platform
The scientific team at ProMab Biotechnologies has developed a completely turnkey CAR T-cell platform, from antibody and hybridoma screening, to lentivirus production, mRNA transfection, and CAR T-cell generation. Antibody humanization, affinity tune-up, and maturation steps are also performed to reduce immunogenicity and improve function and specificity.
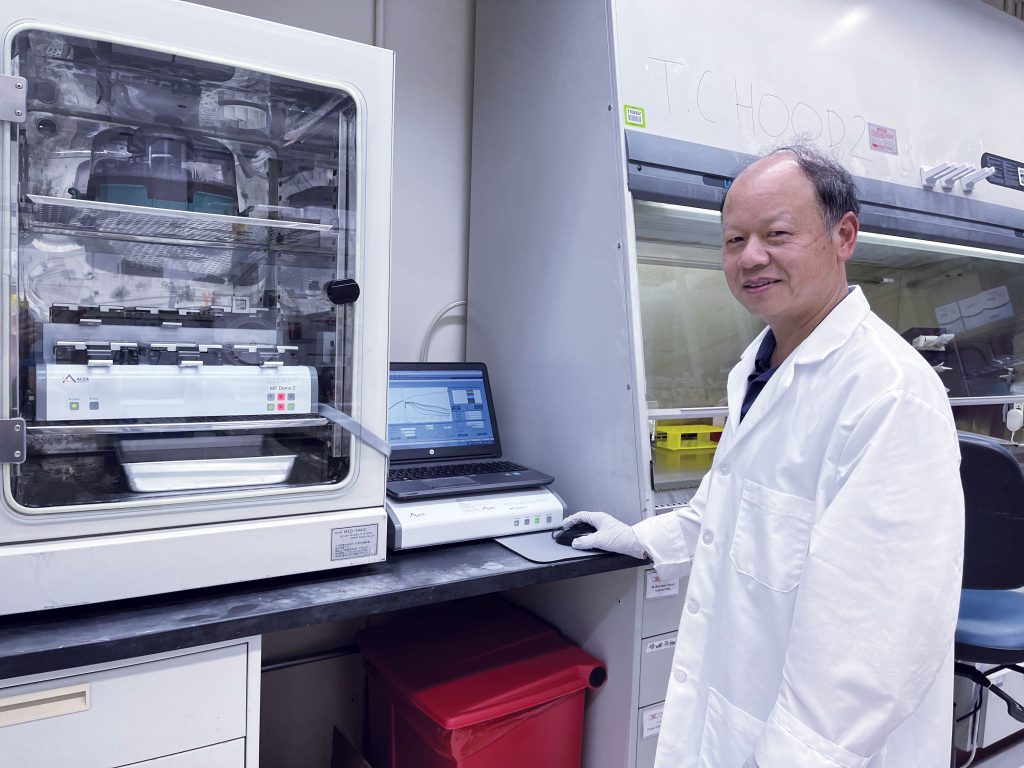
“ProMab Biotechnologies partners with companies that have aggressive timelines. We have adopted several key technologies for our CAR platform that are reliable, efficient, and provide consistent results. We rely heavily on the Agilent NovoCyte Flow Cytometer for antibody screening, detection of the percentage of CAR+ cells, and analysis of CAR T-cell subsets with different markers of T-cell differentiation,” Dr. Golubovskaya states. “The NovoCyte instrument and software are both easy to use, and the system has demonstrated high reproducibility and the ability to simultaneously run many samples, facilitating our high-throughput approach.”
Another critical component of the CAR T-cell platform is a 96-well real-time cytotoxicity assay with the Agilent xCELLigence RTCA instrument, which is used for screening and validation of CAR T-cell efficacy at sensitive effector-to-target ratios. “The advantage of the xCELLigence RTCA is that the data are easily analyzed with the software since killing curves are automatically generated,” Dr. Golubovskaya points out. “After the immune cell killing assay is complete, we can perform 96-well ELISAs for cytokine identification on the supernatants.”
This proven technology has been employed by hundreds of ProMab’s CAR T-cell clients because of the unparalleled insights provided by the real-time CAR-T cell killing data, which helps them to decide which CAR-T cell candidates to advance to the clinic. “The xCELLigence RTCA also saves time—it does not require additional reagents, and the ability to perform statistical analysis at any time point provides a more comprehensive data set in a single run,” Dr. Golubovskaya says. “Most importantly, the in vitro xCELLigence RTCA killing data correlate well with in vivo efficacy data, which helps us accelerate timelines.”
“When we partner with an emerging company that is developing CAR T cells, we suggest using the xCELLigence RTCA system as the best approach to evaluate CAR T-cell killing activity,” Dr. Golubovskaya relates. “We have seen our clients adopt the xCELLigence technology in their own laboratories as they expand their research capabilities.” In addition, the xCELLigence RTCA Software Pro is 21CFR Part 11 compliant, which allows researchers to easily transfer the potency assay to manufacturing.
“Beyond immunophenotyping using NovoCyte Flow Cytometers and immune cell potency screening with xCELLigence RTCA, Agilent provides a comprehensive portfolio of technologies to support various stages of the immune cell therapy development workflow,” says Yama Abassi, PhD, Director of Business Development, Agilent. “Our toolbox of assays enables scientists to fully understand immune cell therapies, from optimizing gene function through gene editing technologies to measuring metabolic pathways to understand immune cell fate and function.”
Watch the Webinar on Demand
“Novel Bispecific CAR-T Cells Against Hematological Cancers” Presented by Vita Golubovskaya, PhD, Director of R&D and Business Development, Promab Biotechnologies
Founded in 2001, ProMab Biotechnologies takes a multi-disciplinary scientific approach to develop and commercialize recombinant proteins, antibodies, CAR T-cells, CAR NK cells, and other engineered cell lines using high-throughput technologies. Proprietary products, in addition to services, are provided to the global biomedical research community through collaborations, partnerships, and joint ventures with biotechnology companies.
About Agilent xCELLigence RTCA Instruments
The Agilent xCELLigence Real-Time Cell Analysis (RTCA) instruments use label-free cellular impedance to continuously monitor cell behavior with high sensitivity and reproducibility. The instruments operate in a standard CO2 cell culture incubator. Simply plate cells and obtain real-time kinetic data. Data acquisition and analysis are easy to perform using RTCA Software Pro, which also supports FDA 21 CFR Part 11 compliance. The xCELLigence RTCA eSight model combines impedance with live-cell imaging for
increased confidence in cell analysis and conclusions.
About Agilent NovoCyte Flow Cytometers
Agilent NovoCyte Flow Cytometers offer excellent capabilities, high-quality data, and an easy-to-use platform to save researchers time when acquiring and analyzing experiments. They provide an expanded set of capabilities that accommodate today’s high-end and increasingly sophisticated multicolor flow cytometry assays. Choose from 1 to 5 lasers with up to 30 state-of-the-art fluorescence detection channels. The intuitive and industry-leading NovoExpress software has been further advanced, providing an exceptional user experience in data acquisition, analysis, and reporting.
For Research Use Only. Not for use in diagnostic procedures.
References
1. Chong EA, Ruella M, Schuster SJ: Five-year outcomes for refractory B-cell lymphomas with CAR T-cell therapy. N Engl J Med 384:673-674, 2021.
2. Samur, M.K., Fulciniti, M., Aktas Samur, A. et al. Biallelic loss of BCMA as a resistance mechanism to CAR T cell therapy in a patient with multiple myeloma. Nat Commun 12, 868 (2021).
3. Golubovskaya et al. Novel CS1 CAR-T cells and bispecific CS1-BMAC-CAR-T cells effectively target multiple myelomas. Biomedicines (2021), 9, 1422.
4. Golubovskaya V, Zhou H, Li F, et al. Novel CD37, Humanized CD37 and Bi-Specific Humanized CD37-CD19 CAR-T Cells Specifically Target Lymphoma. Cancers (Basel). 2021;13(5):981. Published 2021 Feb 26. doi:10.3390/cancers13050981