For some time now, researchers and clinicians have known about significant disparities in cancer survival outcomes that are incumbent upon the patient’s sex. Moreover, patients with cancers stemming from non-reproductive organs, such as bladder and liver cancer, have striking discrepancies in incidence, progression, and response to treatment. Yet, in almost all cases, male patients have worse prognoses and outcomes—a phenomenon that has puzzled the scientific community for decades.
Thankfully, a new study led by researchers in the Pelotonia Institute for Immuno-Oncology (PIIO) at The Ohio State University Comprehensive Cancer Center—Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James)—examined the differences in intratumoral immune responses between male and female cancers of non-reproductive origin. Findings from the new study were published recently in Science Immunology through an article entitled “Androgen conspires with the CD8+ T cell exhaustion program and contributes to sex bias in cancer.”
The focus of this research was the T cell immune response to malignancy, a key determinator of outcomes in cancer and an important target that has contributed to the renaissance of cancer immunotherapy seen in recent years. The study reported a landmark finding describing how male sex hormones contribute to cancer-related sex bias via the modulation of CD8+ T cells—a population of cells often referred to as cancer “killer” cells, which mediate adaptive immunity and are critical for mounting an anti-tumor response.
“Collectively, these findings highlight androgen-mediated promotion of CD8+ T cell dysfunction in cancer and suggest broader implications for therapeutic development to address sex disparities in health and disease,” explained senior study investigator Zihai Li, MD, PhD, a cancer immunologist, medical oncologist, and founding director of the PIIO at OSUCCC—James.
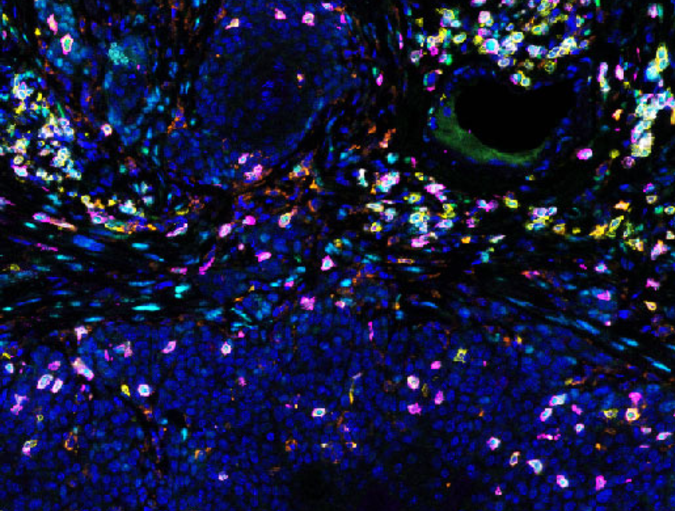
Androgens are sex hormones more highly present in males. This study revealed that CD8+ T cells from cancers in male subjects, including human patients and mice, are more likely to have characteristics of a weakened anti-tumor immune function, also known as “exhausted” T cells. Androgen signaling promotes the progenitor exhausted CD8+ T cell phenotype via modulating the expression of TCF1, a master regulator of CD8+ T cell function.
“We established a role for CD8+ T cell-dependent anti-tumor immunity in mediating sex differences in tumor aggressiveness, which is driven by the gonadal androgen but not sex chromosomes. A male bias exists in the frequency of intratumoral antigen-experienced Tcf7/TCF1+ progenitor exhausted CD8+ T cells that are devoid of effector activity as a consequence of intrinsic androgen receptor (AR) function,” the authors wrote. “Mechanistically, we identified a novel sex-specific regulon in progenitor exhausted CD8+ T cells and a pertinent contribution from AR as a direct transcriptional trans-activator of Tcf7/TCF1. The T cell-intrinsic function of AR in promoting CD8+ T cell exhaustion in vivo was established using multiple approaches, including loss-of-function studies with CD8-specific Ar knockout mice. Moreover, ablation of the androgen-AR axis rewires the tumor microenvironment to favor effector T cell differentiation and potentiates the efficacy of anti-PD-1 immune checkpoint blockade.