Scientists at Tufts University have developed a low cost, “smart” bandage that can monitor wounds and automatically deliver antibiotic drugs to the wound site. Measuring less than 3 mm thick, the prototype bandage contains the latest flexible electronic components, including embedded sensors that measure pH and temperature. The readings are then fed to an onboard microprocessor that analyzes the data and, if there is any sign of infection, triggers the release of antibiotics.
Headed by Sameer Sonkusale, Ph.D., a professor of electrical and computer engineering at Tufts University’s School of Engineering, the team describes the bandage in the journal Small. “The smart bandage we created with pH and temperature sensors and antibiotic drug delivery is really a prototype for a wide range of possibilities,” Dr. Sonkusale comments. The researchers’ published paper is entitled, “Smart Bandage for Monitoring and Treatment of Chronic Wounds.”
Chronic, non-healing skin wounds resulting from trauma such as burns or from diseases such as diabetes affect more than 25 million people in the U.S. and, according to one report, result in an estimated $28 billion in Medicare costs every year. Typically treated at home or in an outpatient setting, chronic wounds are prone to infection, and are the leading cause of nontraumatic limb amputations worldwide, the authors write.
Administering treatment at the right time can help healing but, as the researchers point out, “This approach requires real-time monitoring of the wound environment with on-demand drug delivery in a closed-loop manner.” Many patients with chronic wounds are elderly and non-ambulatory, and would also have trouble self-administering treatment.
The team has now taken advantage of the latest electronic components to develop a new type of bandage that can not only monitor the wound environment in real time, but also dispense drugs in response to key wound cues. “We've been able to take a new approach to bandages because of the emergence of flexible electronics,” says Dr. Sonkusale. “In fact, flexible electronics have made many wearable medical devices possible, but bandages have changed little since the beginnings of medicine. We are simply applying modern technology to an ancient art in the hopes of improving outcomes for an intractable problem.”
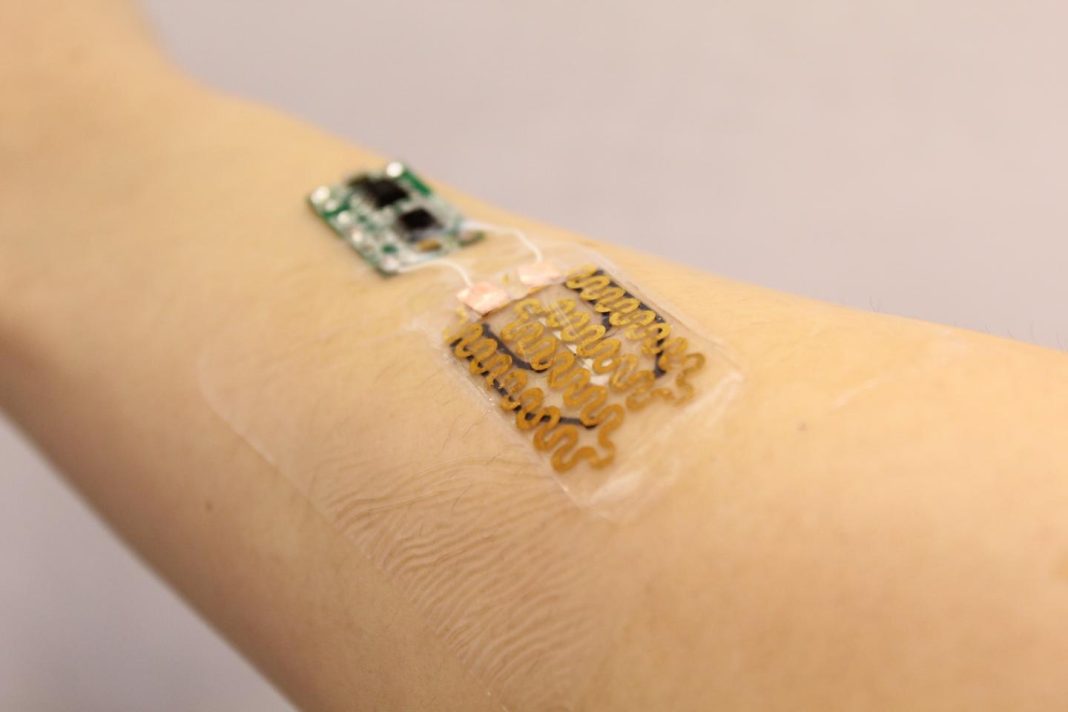
The prototype bandage comprises heating elements and a thermoresponsive drug carrying gel that can be heated to release its drug cargo directly to the wound site. Drug release is triggered by a microprocessor, also carried in the bandage, which analyzes pH and temperature data transmitted by flexible, embedded sensors. pH, for example, is a key parameter for monitoring infection. Wounds that are healing normally typically have a pH of 5.5-6.5, but the pH may rise when wounds become infected. Similarly, changes in temperature in and around the wound environment can indicate when there is inflammation.
The complete unit is attached to a transparent medical tape. The researchers chose components that would help keep the bandage low cost and disposable, except for the microprocessor, which can be re-used. And while the current prototype incorporates sensors that measure pH and temperature, the team has also developed flexible sensors for measuring oxygenation, and envisage the use of biosensors for detecting specific biomarkers. “One can imagine embedding other sensing components, drugs, and growth factors that treat different conditions in response to different healing markers,” Dr. Sonkusale notes.
The team has evaluated the bandage under in vitro conditions, and preclinical testing is now underway to determine how well it can help chronic wounds to heal, in comparison with traditional bandage and wound care products. “This flexible, smart wound dressing has the potential to significantly impact the treatment of chronic wounds,” the authors conclude.