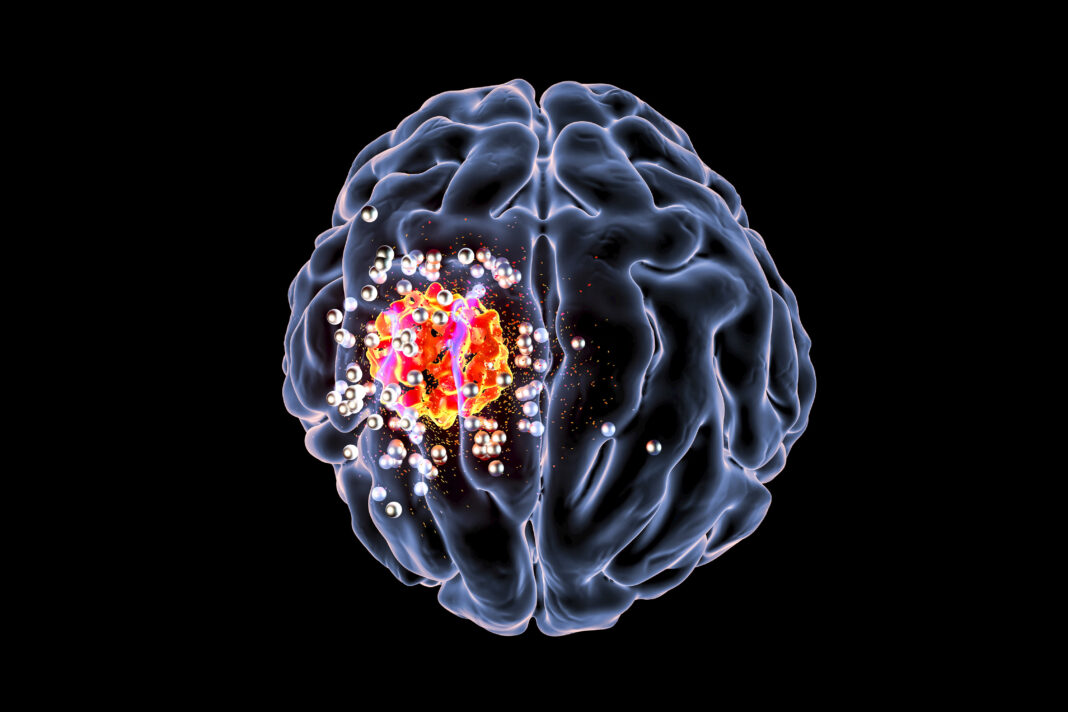
Researchers at Mount Sinai Health System and Memorial Sloan Kettering Cancer Center have developed a new drug delivery approach that uses nanoparticles to enable more effective and targeted delivery of anticancer drugs to treat brain tumors in children.
The fucoidan-based nanoparticle technology allows for the enhanced delivery of anticancer drugs across the blood-brain barrier (BBB) to the specific locations of brain tumors, while sparing normal brain regions. Tests in mice showed that nanoparticle delivery improved the effectiveness and reduced the toxicities of the anticancer drug vismodegib.
“We show that we can more successfully deliver lower doses of the drug in a more effective manner to the specific sites of tumor within the brain, while sparing the bone toxicity that is seen in younger patients,” said Praveen Raju, MD, PhD, Co-Director of the Children’s Brain and Spinal Tumor Center at Mount Sinai Kravis Children’s Hospital. Raju is co-senior author of the team’s study, which is published in Nature Materials, and titled “P-selectin-targeted nanocarriers induce active crossing of the blood–brain barrier via caveolin-1-dependent transcytosis.” In their paper the researchers concluded, “… we report an active mechanism of transendothelial transport that can be exploited to improve drug delivery across activated brain endothelial cells at sites of intracranial disease in conditions with an intact BBB … Overall, these findings demonstrate a potent strategy for targeted intracranial pharmacodelivery that overcomes the restrictive blood–brain barrier to achieve enhanced tumour-selective penetration and has therapeutic implications for diseases within the central nervous system.”
Medulloblastoma is the most common malignant pediatric brain tumor, accounting for about 20% of all brain tumors in children. It is highly aggressive, difficult to treat, and considered incurable in nearly 30% of patients. Even children who are treated successfully may experience severe long-term disabilities and health issues, primarily due to the adverse side effects of radiation and chemotherapy. In about a third of cases this form of brain tumor is mediated by Sonic hedgehog signalling, the authors noted.
Site-directed drug delivery to the affected brain tissue is “an elusive goal” that is hindered by a distinct and highly regulated blood-brain barrier, which normally protects the brain from infections or other harmful substances. “… the integrity of the BBB can considerably impact treatment efficacy,” the investigators wrote. “This is well evidenced in medulloblastoma wherein patients in the Sonic hedgehog medulloblastoma subgroup (SHH-MB) suffer worse clinical outcomes due, in part, to an intact BBB limiting the entry of drugs into the brain at therapeutic concentrations.”
Given the difficulties in getting small molecule compounds across the BBB, researchers have turned to nanoparticles as a potential approach to improve drug delivery to brain tissues. However, there have been challenges with existing, passive approaches to transporting drug-loaded nanoparticles across the intact, or compromised BBB. For their newly reported study, the researchers made use of a normal mechanism that the immune system uses to traffic white blood cells to sites of infection, inflammation, or tissue injury.
Rather than randomly sending immune cells throughout the body, there is a homing mechanism on activated blood vessels that immune cells use to go where they are needed. The researchers used this unique homing feature, which is also found within brain tumor blood vessels, to target their drug-loaded fucoidan-based nanoparticles to the site of the disease and not the normal brain regions. “In this study, we investigated active transcellular transport mechanisms to enhance drug delivery across an intact BBB specifically to brain tumour tissue,” they commented.
Using the new drug delivery platform in a genetically relevant mouse model of medulloblastoma, the research team was able to enhance the efficacy of an anticancer drug, vismodegib, that could potentially be useful for a subset of medulloblastoma patients, but which is currently limited by the bone toxicity it secondarily creates in children. “… targeted inhibition of the SHH effector Smoothened (SMO) via vismodegib causes premature bone growth plate fusion in paediatric patients, probably as a result of the high doses required for therapeutic efficacy,” the explained. In contrast, the team noted, “Fucoidan nanoparticles encapsulating the Smoothened inhibitor vismodegib (FiVis) exhibited potent effector inhibition at low drug doses, striking antitumour efficacy and attenuated on-target bone-related toxicities.”
“In addition, we showed that this targeted drug delivery approach is further enhanced with very-low-dose radiation, which is a standard therapy already used for most children and adults with primary and metastatic brain tumors,” said Raju, associate professor of neurology, neuroscience, and pediatrics at Icahn School of Medicine at Mount Sinai. The authors further noted, “Using a genetic mouse model of SHH-MB with an intact BBB, we found that P-selectin targeting results in active transport in tumor endothelium to enable delivery of fucoidan-based nanoparticles selectively into the tumour microenvironment, which is enhanced by RT.”
Raju continued, “Importantly, our blood-brain barrier drug delivery approach has the potential to improve the delivery of drugs for other pediatric brain tumors and localized diseases in the brain in both children and adults, including focal epilepsy, multiple sclerosis, stroke, and possibly neurodegenerative disorders.”
Co-senior author Daniel Heller, PhD, Head of the Cancer Nanomedicine Laboratory and Member in the Molecular Pharmacology Program at Memorial Sloan Kettering Cancer Center, added “Certain proteins appear on blood vessels at sites of inflammation that help white blood cells exit the bloodstream. They work like police officers at the site of a car accident, who let in emergency personnel to help. We sent in our own emergency personnel, in the form of drug-loaded nanoparticles, composed of certain sugar molecules that can target these same proteins.”
The researchers anticipate that continued investigation and development of this method to harness and improve the transport of materials across the blood-brain barrier and other sites will be instrumental for improving the efficacy of several classes of approved and experimental therapeutics.
This drug delivery platform can be used to treat cancers in the brain and other sites of the body, as well as other inflammation-related diseases in the central nervous system and elsewhere.
Raju and his colleagues were recently awarded $2.8 million from the National Institutes of Health to dissect the mechanism of medulloblastoma tumor cell maturation and to identify targets to induce differentiation therapeutically using high-resolution genomics and epigenetics techniques and this new blood-brain barrier penetrating drug delivery platform.
Raju was also recently awarded a ChadTough Defeat DIPG Foundation Game Changer Grant of $600,000 that will support research into using this drug delivery approach for diffuse intrinsic pontine glioma (DIPG), a difficult-to-treat pediatric brain tumor localized to the pons, a part of the brain stem. Oren Becher, MD, Chief of the Jack Martin Fund Division of Pediatric Hematology-Oncology, the Steven Ravitch Chair in Pediatric Hematology-Oncology, and Professor of Pediatrics at Icahn Mount Sinai, is collaborating in that research.