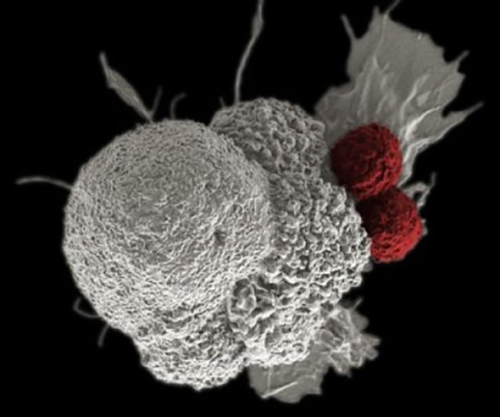
![Researchers have developed a new strategy to maximize the effectiveness of anticancer immune therapy. [NCI]](https://genengnews.com/wp-content/uploads/2018/08/160919121945_1_540x3606622019858-1.jpg)
Researchers have developed a new strategy to maximize the effectiveness of anticancer immune therapy. [NCI]
Exploiting the body’s immune system to fight progressive pathological conditions such as cancer, Crohn’s, and Alzheimer’s is the basis for novel immunotherapy compounds that are beginning to take the drug market by storm. While various immunotherapy regimens have met with excellent results, not every patient has had an efficacious response. Now, researchers at the University of California San Diego School of Medicine and Moores Cancer Center have just identified a strategy that they believe will maximize the effectiveness of anticancer immune therapy.
“Immunotherapies, such as T-cell checkpoint inhibitors, are showing great promise in early treatments and trials, but they are not universally effective,” explained senior study investigator Judith Varner, Ph.D., professor in the departments of pathology and medicine at UC San Diego School of Medicine. “We have identified a new method to boost the effectiveness of current immune therapy. Our findings also improve our understanding of key mechanisms that control cancer immune suppression and could lead to the development of more effective immunotherapies.”
In the new study— the findings of which were published recently in Nature in an article entitled “PI3Kγ Is a Molecular Switch That Controls Immune Suppression”—the research team identified a molecular switch that controls immune suppression, opening the possibility to further improve and refine emerging immunotherapies that boost the body's own abilities to fight disease.
The initial response by the immune system, in response to pathogens, injury, or disease, typically comes from macrophages, white blood cells that express proinflammatory cytokines that, in turn, activate T cells to attack the health threat. The macrophages then switch gears to express other cytokines that dampen T-cell activation, stimulating tissue repair.
For chronic inflammatory diseases such as Alzheimer's and Crohn's, however, macrophages associated with the malignancy continue to produce proinflammatory cytokines and other substances that kill or transform healthy cells. In cancer, highly abundant macrophages express anti-inflammatory cytokines that induce immune suppression, effectively stopping the healing process.
“Recently developed cancer immunotherapeutics, including T-cell checkpoint inhibitors and vaccines, have shown encouraging results in stimulating the body's own adaptive immune response,” noted co-author Ezra Cohen, M.D., professor of medicine at UCSD and associate director of Moores Cancer Center. “But they are effective only for a subset of patients, probably because they do not alter the profoundly immunosuppressive microenvironment created by tumor-associated macrophages. Our work offers a strategy to maximize patient responses to immune therapy and to eradicate tumors. “
“We show that macrophage PI(3)Kinase γ controls a critical switch between immune stimulation and suppression during inflammation and cancer,” the authors wrote. “PI3Kγ signaling through Akt and mTor inhibits NFκB activation while stimulating C/EBPβ activation, thereby inducing a transcriptional program that promotes immune suppression during inflammation and tumor growth. In contrast, selective inactivation of macrophage PI3Kγ stimulates and prolongs NFκB activation and inhibits C/EBPβ activation, thus promoting an immunostimulatory transcriptional program that restores CD8+ T cell activation and cytotoxicity and synergizes with checkpoint inhibitor therapy to promote tumor regression and extend survival in mouse models of cancer.”
The current study builds upon previous work from Dr. Varner’s lab, in which the researchers reported that blocking PI3Kγ in tumor-associated macrophages stimulated the immune response and inhibited tumor cell invasion, metastasis, and fibrotic scarring caused by pancreatic ductal adenocarcinoma (PDAC) in animal models.
Interestingly, in humans, PDAC is the most common malignancy of the pancreas—being extremely aggressive and difficult to treat. Though only the 12th most common type of cancer in the United States, pancreatic cancer is the fourth most common cause of cancer-related death.
“PDAC has one of the worst 5-year survival rates of all solid tumors, so new treatment strategies are urgently needed,” remarked lead study author Megan Kaneda, Ph.D., assistant project scientist in Dr. Varner's laboratory.
Combining all of the current information suggests that therapeutic targeting of immune system signaling pathways, which regulate the switch between macrophage polarization states, governs immune suppression in cancer and other disorders.