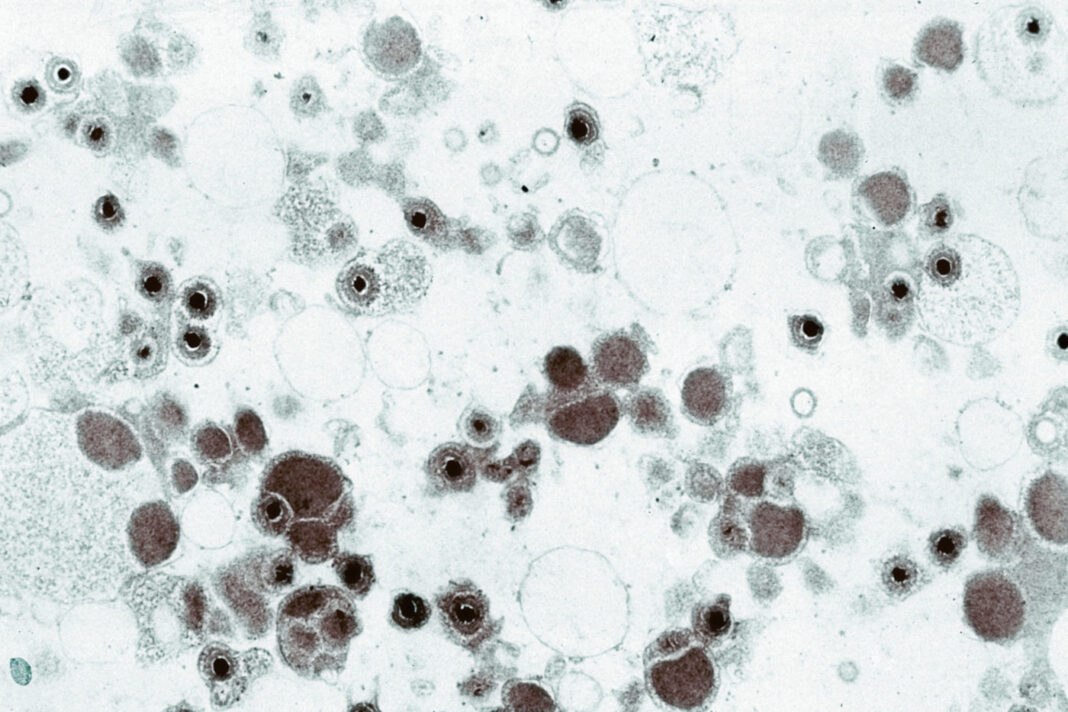
A Duke Health-led research team says it has identified a key marker that will help speed effective vaccine designs for cytomegalovirus (CMV), the most common congenital infection worldwide and a leading cause of infant brain damage.
In a study “Antibody binding to native cytomegalovirus glycoprotein B predicts efficacy of the gB/MF59 vaccine in humans” appearing online Science Translational Medicine, the researchers describe an immune surrogate that demonstrates when a vaccine has elicited the necessary antibodies that protect against CMV infection. The finding is already being applied to screen potential vaccines.
“Human cytomegalovirus (CMV) is the most common infectious cause of infant brain damage and posttransplant complications worldwide. Despite the high global burden of disease, vaccine development to prevent infection remains hampered by challenges in generating protective immunity. The most efficacious CMV vaccine candidate tested to date is a soluble glycoprotein B (gB) subunit vaccine with MF59 adjuvant (gB/MF59), which achieved 50% protection in multiple historical phase 2 clinical trials,” write the investigators.
“The vaccine-elicited immune responses that conferred this protection have remained unclear. We investigated the humoral immune correlates of protection from CMV acquisition in populations of CMV-seronegative adolescent and postpartum women who received the gB/MF59 vaccine. We found that gB/MF59 immunization elicited distinct CMV-specific immunoglobulin G (IgG)–binding profiles and IgG-mediated functional responses in adolescent and postpartum vaccinees, with heterologous CMV strain neutralization observed primarily in adolescent vaccinees.”
“Using penalized multiple logistic regression analysis, we determined that protection against primary CMV infection in both cohorts was associated with serum IgG binding to gB present on a cell surface but not binding to the soluble vaccine antigen, suggesting that IgG binding to cell-associated gB is an immune correlate of vaccine efficacy. Supporting this, we identified gB-specific monoclonal antibodies that differentially recognized soluble or cell-associated gB, revealing that there are structural differences in cell-associated and soluble gB are relevant to the generation of protective immunity. Our results highlight the importance of the native, cell-associated gB conformation in future CMV vaccine design.”
“CMV has been recognized as a top priority for vaccine development for more than 20 years, yet we remain without an approved vaccine. This work provides a way to assure that current and future vaccine candidates stimulate an effective immune response,” said senior author Sallie Permar, MD, a professor in the departments of Pediatrics, Immunology, Molecular Genetics and Microbiology, and Pathology at Duke University School of Medicine.
“We are beyond due for vaccines to be developed to protect against this virus, which infects 40,000 infants a year in the United States alone, with a third of these children developing permanent hearing loss, brain damage or neuro-developmental delays,” Permar added.
Permar and colleagues, including lead author Jennifer A. Jenks, an MD/PhD candidate at Duke, investigated the immune responses that protected against CMV infections in women who received the investigational protein vaccine gB/MF59. The main component of this vaccine was the CMV protein “gB,” which the virus uses to enter human cells.
The investigational vaccine was expected to generate an immune response that could stop CMV from entering host cells. It was about 50% effective in preventing CMV infection in multiple Phase 2 clinical trials, but an acceptable CMV vaccine should be at least 70% effective.
The researchers found that protection against CMV infection was associated with the presence of antibodies in the blood that bind to the target protein gB when it is presented on a cell surface, but not to gB when it is in its soluble, free-floating form used in the gB/MF59 vaccine.
This finding suggests that future CMV vaccines should be designed to target the appropriate conformation of gB. Additionally, the researchers report, the presence of these antibodies may be used to predict the potential efficacy of future candidate vaccines.
“This is an important immunologic endpoint for vaccine development and evaluation,” Jenks said. “This could serve as a surrogate for assessing antiviral function and could aid in vaccine evaluation in preclinical and early-phase clinical trials.”