![A vaccine-like approach to prevent atherosclerotic heart disease looks promising after a recent paper shows that it has a cholesterol- and inflammation-lowering effect in a mouse model. This image shows a cross-section of a mouse aortic blood vessel in a mouse immunized with AT04A, a peptide-based formulation that raises antibodies against PCSK9, an endogenous protein that interferes with cholesterol clearance. Notice that the vessel appears to have little or no plaque. [The Netherlands Organization of Applied Scientific Research]](https://genengnews.com/wp-content/uploads/2018/08/Jun20_2017_NetherlandsOrgAppliedScientificResearch_CrossSectionMouseAorticBloodVessel2301891587-1.jpg)
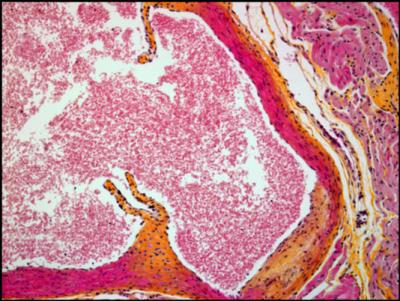
A vaccine-like approach to prevent atherosclerotic heart disease looks promising after a recent paper shows that it has a cholesterol- and inflammation-lowering effect in a mouse model. This image shows a cross-section of a mouse aortic blood vessel in a mouse immunized with AT04A, a peptide-based formulation that raises antibodies against PCSK9, an endogenous protein that interferes with cholesterol clearance. Notice that the vessel appears to have little or no plaque. [The Netherlands Organization of Applied Scientific Research]
It gives rise to antibodies that could prevent disease, but it’s not quite a vaccine. It qualifies as an immunotherapy because it targets one of the body’s own proteins, not a protein associated with a pathogen. The “it” in this case is AT04A, a peptide-based formulation that induces an immune response against a protein that interferes with cholesterol clearance.
According to a recent study, AT04A lowered cholesterol in a mouse model of atherosclerosis. This result, detailed June 19 in the European Heart Journal, is an encouraging sign that AT04A may also perform well in humans. A Phase I study is, in fact, currently under way. If this study establishes that AT04A is both active and safe, it will encourage further evaluations, which may culminate in the development of effective treatments to prevent cardiovascular disease.
The mouse study (“The AT04A Vaccine against Proprotein Convertase Subtilisin/Kexin Type 9 Reduces Total Cholesterol, Vascular Inflammation, and Atherosclerosis in APOE*3Leiden.CETP Mice”) is the first to show that it is possible to immunize genetically modified mice with a molecule that causes the body to produce antibodies against an enzyme called PCSK9 (proprotein covertase subtilisin/kexin type 9), which plays a role in preventing the clearance of low-density lipoprotein cholesterol (“bad” cholesterol) from the blood.
The AT04A vaccine induced high and persistent antibody levels against PCSK9, causing a significant reduction in plasma total cholesterol and bad cholesterol compared with controls.
“Plasma inflammatory markers such as serum amyloid A (SAA), macrophage inflammatory protein-1β (MIP-1β/CCL4), macrophage-derived chemokine (MDC/CCL22), cytokine stem cell factor (SCF), and vascular endothelial growth factor A (VEGF-A) were significantly diminished in AT04A-treated mice,” reported the authors of the European Heart Journal article. “As a consequence, treatment with the AT04A vaccine resulted in a decrease in atherosclerotic lesion area…and aortic inflammation as well as in more lesion-free aortic segments.”
When the AT04A formulation was injected under the skin in mice that have been fed fatty, Western-style food, it reduced the total amount of cholesterol by 53%, shrank atherosclerotic damage to blood vessels by 64%, and reduced biological markers of blood vessel inflammation by 21% to 28%, compared to unvaccinated mice. Furthermore, the induced antibodies remained functional over the whole study period, and concentrations were still high at the end of the study.
“The reduction in total cholesterol levels was significantly correlated with induced antibody concentration, proving that induced antibodies caused the reduction in cholesterol and also are ultimately responsible for the reduction of atherosclerosis development,” noted Günther Staffler, Ph.D., chief technology officer at AFFiRis (the company that developed AT04A) and one of the authors of the study. “As antibody concentrations remained high at the end of the study, it can be assumed they would continue to reduce cholesterol levels for some time afterwards, resulting in a long-lasting effect, as has been shown in previous studies.
“If these findings translate successfully into humans, this could mean that, as the induced antibodies persist for months after a vaccination, we could develop a long-lasting therapy that, after the first vaccination, just needs an annual booster. This would result in an effective and more convenient treatment for patients, as well as higher patient compliance.”
At present, drugs such as statins can be used to lower low-density lipoprotein cholesterol (LDL-C), but they have to be taken on a daily basis and, although they are generally well tolerated, they can cause adverse side effects in some people. The most recently approved cholesterol-lowering compounds are monoclonal antibodies targeting PCSK9, which are highly effective, but their effect is short-lived, resulting in frequent reapplication and high costs.
PCSK9, however, may be targeted via an alternative approach, the one evaluated in the current study. The enzyme PCSK9 is made in the liver and it locks on to LDL-C receptors, reducing the ability of these receptors to get rid of LDL-C from the blood. When injected, AT04A causes the body to produce antibodies that block the function of PCSK9, so that the activity of the LDL-C receptors is increased.
“The way that AT04A is administered is comparable to a vaccine,” explained Dr. Staffler. “However, the difference between a conventional vaccine and our approach is that a vaccine induces antibodies that are specific to bacterial or viral proteins that are foreign to the body—pathogens—whereas AT04A induces antibodies against a target protein that is produced by the body—endogenous proteins. This it is really an immunotherapeutic approach rather than a vaccine approach.”
In 2015, a Phase I clinical study started at the department of clinical pharmacology, Medical University of Vienna, Austria, studying AT04A and another molecule, AT06A, in 72 healthy people to assess its safety and activity. The study is expected to complete at the end of this year.
In an accompanying editorial (“Vaccination to Prevent Atherosclerotic Cardiovascular Disease”) in the European Heart Journal, Prof. Ulrich Laufs, of the University of Leipzig, Germany, and Prof. Brian Ference, of the University of Bristol, U.K., and the Wayne State University School of Medicine, Detroit, MI, commented as follows: “It appears promising to further evaluate long-term LDL-C lowering by vaccination against PCSK9 for the prevention of atherosclerotic events.” However, they added that “safety, the response in humans and the very important but unknown long-term immune effects need to be very carefully addressed during the course of clinical development.”
In particular, reductions in total cholesterol via statins and other drugs are associated with an increase in new-onset diabetes. “Therefore,” the editorial continued, “one potential safety concern for long-term lowering of LDL-C with a vaccine directed against PCSK9 is the potential for an increased risk of new-onset diabetes. In the short term, the LDL-C-lowering effect of statins and PCS9 inhibitors appears to far outweigh the risks of new-onset diabetes.”