When you’re trying to solve a puzzle, having all the pieces isn’t enough. You need a strategy. For example, if you want to complete a jigsaw puzzle, you’ll probably begin by piecing together its edges. More challenging puzzles, such as those encountered in drug development, require strategies that are rather more sophisticated. Indeed, in drug development, the strategic challenges are so involved that they often prompt biotechnology and biopharmaceutical companies to secure the services of a contract research organization, or CRO.
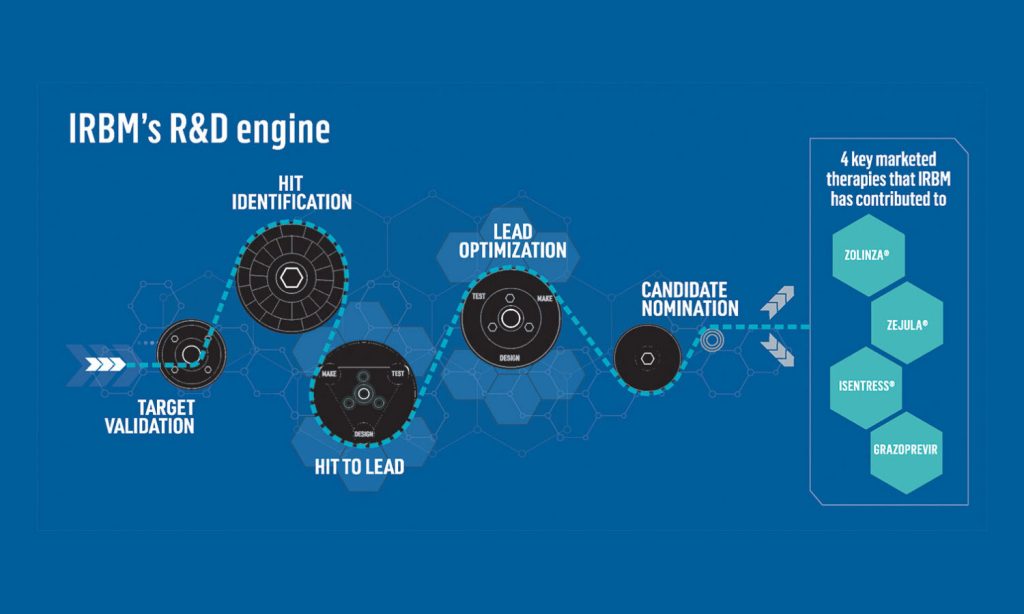
The CRO known as IRBM advocates what it calls an integrated approach. This approach, IRBM explains, is all about pulling together technologies to enable target identification, candidate screening, biomarker development, in vivo testing, and clinical development. What’s more, IRBM emphasizes the importance of having a vision. What good is piecing together a border or frame if one cannot see the big picture?
In drug development, envisioning the big picture is equivalent to knowing how to exploit fundamental biological insights and move toward the ultimate goal: a safe and effective drug. Moreover, it is desirable to achieve this goal with all deliberate speed.

Vice President and Head of North American Business Development, IRBM
IRBM argues that in drug development, speed is about cultivating collaborative relationships. These are relationships in which data is shared freely among drug development partners, enabling data-driven workflows. To explain how these relationships form the basis of strategic drug development efforts, two IRBM executives, Alberto Bresciani and Michele Luche, agreed to an exclusive interview with GEN magazine. Bresciani is IRBM’s director of high-throughput biology and screening, and Luche is the CRO’s vice president and head of North American business development.
“In drug discovery and development programs,” Bresciani and Luche agree, “it is necessary to address questions about fundamental biology and optimal therapeutic modality, and to find answers using advanced methods and data-driven decisions.” Bresciani and Luche maintain that IRBM is able to ask the right questions and find the right answers because it “has expertise in imaging, in structural biology, in evaluating molecules in primary cell lines, and in using stem cells, 3D cell cultures, and co-cultures that support disease-relevant systems.” Besides noting that IRBM employs technologies that offer better spatial and temporal resolution, Bresciani and Luche emphasize that the CRO can accelerate drug discovery by leveraging artificial intelligence and machine learning (AI/ML) technologies and implementing disease-relevant model systems.
Strategic elements
Luche emphasizes the importance of considering targets, goals, model systems, libraries, and liabilities at the outset of the drug discovery program. Doing this makes it easier to identify optimal drug candidates. Luche adds that a high degree of transparency in data sharing between collaborating organizations and within departments in an organization facilitates expediency and high-level strategy in the iterative discovery process. She says, “To have different pieces of the puzzle interact efficiently, reduce cycle times, and leverage powerful collective experience, it’s important that data be promptly reviewed by everybody involved.”
Luche senses that data sharing is becoming more acceptable through the success of collaborative programs. “Traditionally, data was held very close to the chest,” she observes. “Of course, assets should be protected, but we must understand there’s a lot of experience out there that should be harnessed to efficiently bring a candidate to clinic.”
Investing in front-end strategizing, supporting data transparency, and adopting a step-by-step problem-solving approach that incorporates insights from basic biology and AI/ML can be crucial in identifying optimal candidates and terminating suboptimal ones. “Terminating a program is never pleasant, especially if researchers have a personal stake in the project,” Luche relates. “It’s very important that crucial questions are answered quickly via data-driven approaches.”
For example, in the development of proteolysis targeting chimeric (PROTAC) drugs, access to systematic and quantitative assays can be invaluable. If a candidate were to form a ternary complex and bind a target in a biochemical setting, yet fail to degrade the target in cells, such assays could indicate where improvements are needed. “A sequence of assays may be used to test cellular permeability, ternary complex formation, target ubiquitination, and proteasomal delivery and function,” Bresciani details. “These assays can help the design team develop the right solution.”
Under one roof
IRBM believes in the practical merits of maintaining the organization’s capabilities under one roof and applying them to support iterative processes. Short cycle times in complex workflows depend on quick responses and flexibility. Groups looking into biology, chemistry, metabolism, and pharmacokinetics must interact and respond quickly to incoming data.
“Being in the same physical location makes the programs go that much faster,” Luche insists. “You can do research at different locations, but it adds complexity and delays that can be overcome if everybody with a critical role in the program is together.”
Customized systems
A productive strategy at IRBM has been to begin with a modality-agnostic mindset, one that stays focused on basic mechanisms that dictate the development or selection of tools and disease-relevant model systems. “For each target, we develop tailor-made systems,” Bresciani asserts. “Rather than use general libraries to identify hits, we try to understand the biology of the target and ligand, and design ad hoc libraries to maximize our chances.”
For example, IRBM utilizes phage display libraries to identify therapeutic peptides. Phage display, a technology for screening protein interactions at high throughput using bacteriophages, remains one of the most powerful tools for the identification and maturation of protein ligands. IRBM uses phage display to segregate, create, or identify ligands for a target, and to weed out targets with undesirable biological responses.
“We’re fortunate that phage display is part of our broader capabilities in peptide drug discovery to identify high-affinity and high-avidity hits,” Luche notes. “Importantly, it’s not an isolated technology.” When identifying and optimizing candidate peptide drugs for clinical progression, IRBM may draw on a comprehensive array of in vitro and in vivo tools. These tools facilitate studies of various kinds, including pharmacodynamic and pharmacokinetic studies.
AI/ML applications
Traditionally, decisions in drug discovery have depended on expert assessments, linear interpretations of limited data, or intuitive hunches. These counsels are being superseded by AI/ML. By forging new connections between basic biology and decision making, AI/ML can help developers zero in on the best targets, development strategies, and responder populations.
“AI/ML offers testable options based on large training and validation sets,” Bresciani says. “It can present parameters that together [indicate] whether something can be progressed or not.”
Although AI/ML is a powerful technology, it has its limits. “It’s risky,” Bresciani cautions, “to think that AI/ML is applicable under every condition.” The first step to benefiting from AI/ML is understanding when it is appropriate.
For example, AI/ML can be helpful in protein structure–based drug design. AlphaFold-enabled prediction of 3D structure is particularly useful when targets cannot be crystallized, purified directly, or act as disease modulators. Like all tools, Bresciani explains, AlphaFold may be more useful in some contexts than others. He adds that recognizing a suitable context requires that “you have your fundamental biology and the plausibility of your rationale defined.”

In the context of drug discovery, AI/ML often complements traditional approaches instead of replacing them. For example, AI/ML can support a hypothesis-driven approach in drug discovery and evaluate the premises of particular drug discovery projects. “With AI/ML,” Bresciani says, “we can define a target and identify how to measure whether the target is relevant for a certain phenotype, profile, or function.”
Luche also believes AI/ML and basic biology go hand in hand. “Many drugs have been developed because somebody paid attention to a piece of data that wasn’t necessarily on the path but produced a result that warranted follow up,” he explains. “If your AI/ML doesn’t [have a built-in ability to assess] alternative scenarios, you could be missing important things.”
Biomarkers of safety and efficacy
For IRBM, an integrated approach to drug discovery is one that collates all major areas of expertise involved in various therapeutic modalities under one roof. One area of expertise that IRBM prioritizes—and makes a point of employing early in discovery—is biomarker development.
“Biomarkers play a huge role in patient stratification and in characterizing patient responses,” Luche points out. “Where possible, we try to build that into the early discovery phase for all disease areas where it can be useful.” She stresses that early-stage biomarker development is critical in translational research.
Having a biomarker helps in determining how the therapeutic candidate behaves toward its target. It helps identify imaging agents for diagnostics and efficacy estimations. And it helps uncover potential liabilities.
“We start thinking about pharmacodynamic biomarkers when we begin testing target engagement in vitro, long before the discovery process reaches clinical trials,” Bresciani remarks. “We consider how to adapt these biomarkers to measure target engagement in vivo or the primary effect in preclinical and clinical trial stages. This approach can be invaluable for interpretation of results as well as in the identification of the optimal candidate.”
There is a distinct advantage in some of the new therapeutic modalities, such as PROTACs, antisense oligonucleotides, siRNAs, gene therapies, and splicing modulators. The advantage is that the desired pharmacodynamic endpoint is known. “Being able to develop a direct measure of target modulation provides additional information during the discovery and development stages in an in vivo model,” Bresciani explains. “It underpins decisions on dosage, final target levels, and safety.”
Alternative models
In vitro models now include induced pluripotent stem cell–derived blood-brain barrier systems and complex 3D organoid systems. They are gaining popularity in drug development because they can do what animal model systems cannot. Specifically, they can capture the intrinsically human-centric processes that influence and are influenced by certain novel therapeutic modalities.
For example, splicing modulators are a popular new therapeutic modality that are quickly moving from being scientific tools to experimental drugs, based on structure-activity studies. “To test a splicing modulator’s function, you need to have the splicing sites, introns, and exons laid out in a specific way to make it work,” Bresciani notes. With such modulators, testing for on- and certain off-target toxicities may be difficult if animal models are used. In vitro model systems based on human cellular components reserve a predictive advantage.
In the early stages of drug development, the use of in vitro organ-on-chip systems is increasingly common, particularly in certain scenarios. Indeed, the advantages of substituting such systems for animal model systems are beginning to be recognized by regulatory agencies. Whether these advantages should be sought depends on the specific project and the availability of suitable in vivo models.
“The more complex an in vitro system becomes, the more complicated it is to have everything under control to ensure reproducibility,” Bresciani says. “It could take a long time to trust predictions in a new system. For example, we developed a blood-brain barrier system to understand the permeability of compounds and how the barrier responds to the presence of certain drugs. It took us a long time to validate the model.”
Microphysiological model systems such as explant cultures or organoids require extensive testing and validation under stringently controlled conditions before they gain acceptance as reliable models for efficacy and safety studies. Bresciani states, “Regulatory agencies are already evaluating such in vitro organoid or 3D culture systems in scenarios where animal models cannot be predictive due to the lack of underlying biology for a specific intervention.” Such systems may be easier to use in efficacy tests than in safety tests, as the former involve confirming the activity of molecules under specific conditions in a disease-relevant system.

