![New evidence suggests that a microscopic fungus called <i>Candida tropicalis</i> triggered gut inflammation and exacerbated symptoms of Crohn’s disease. [NIH]” /><br />
<span class=](https://genengnews.com/wp-content/uploads/2018/08/crohndiseaseulcerativecolitis6981242156-1.jpeg) New evidence suggests that a microscopic fungus called Candida tropicalis triggered gut inflammation and exacerbated symptoms of Crohn’s disease. [NIH]
New evidence suggests that a microscopic fungus called Candida tropicalis triggered gut inflammation and exacerbated symptoms of Crohn’s disease. [NIH]
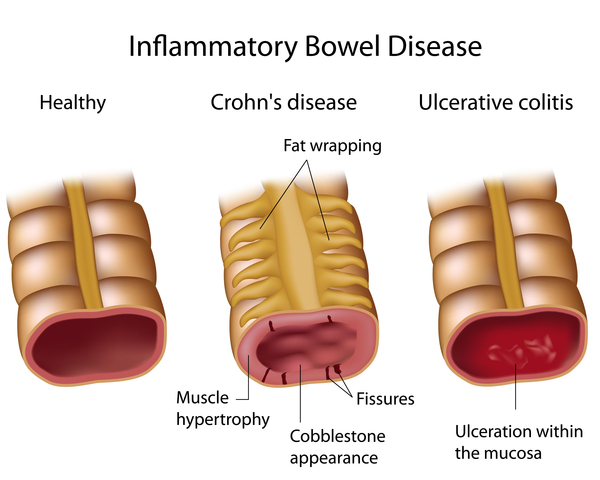
Inflammatory bowel disease (IBD) affects millions worldwide and can often lead to serious intestinal disorders if left unchecked. While there has been a wave of IBD drugs that have recently come to market, the underlying molecular mechanisms for many of these disorders remains a mystery. Now, a team of researchers at Case Western Reserve University (CWRU) School of Medicine recently presented new data at the Digestive Disease Week conference in Chicago showing that the fungus Candida tropicalis triggers gut inflammation and exacerbates symptoms of Crohn's disease. Data from the study were presented in a talk entitled “Infection with the Fungus Candida Tropicalis Significantly Increases the Severity of Colitis in C57bl/6 Mice.”
“The type of microorganisms that live in our intestine, our microbiome, has been shown to be a key element for triggering Crohn's disease,” explained lead study investigator Luca Di Martino, Ph.D., a postdoctoral research fellow in the Digestive Health Research Institute at CWRU School of Medicine. “Recent studies have shown that the abundance of the fungus Candida tropicalis is significantly higher in the intestine of Crohn's disease patients compared to healthy people.” Di Martino investigated how C. tropicalis and other gut microorganisms may influence intestinal inflammation.
Colon inflammation, or colitis, is a painful yet common symptom in Crohn's disease and many scientists believe colitis is caused by an abnormal immune response during which the body tries to fight an infection—attacking the intestinal tract at the same time. The CWRU researchers set out to prove that C. tropicalis infection can intensify this malfunction.
In the current study, the CWRU researchers induced colitis symptoms in mice by adding low levels of dextran sodium sulfate to mice drinking water. The chemical causes acute intestinal injury, similar to a colitis flare. Next, they infected a subset of the mice with C. tropicalis fungi and examined the mouse intestinal tracts and gut bacteria.
The investigators discovered that mice infected with C. tropicalis fungi had intensified Crohn's disease symptoms, compared to uninfected mice—suggesting that antifungal medications could combat debilitating symptoms of the disease by lowering gut levels of C. tropicalis. Moreover, the researchers suggested that C. tropicalis fungus may trigger gut inflammation by modulating levels of other gut bacteria.
“We found that high levels of C. tropicalis increases the abundance of harmful proteobacteria in the intestine, such as E. coli, disrupting the normal balance of the gut bacteria and creating a dysbiosis, a key element that triggers intestinal inflammation,” Dr. Di Martino remarked. “There was a significantly higher abundance of proteobacteria, the same type of deleterious bacteria found increased in Crohn's patients. This confirmed that the presence and the abundance of fungi in the intestine have the ability to modify the bacteria living in our intestine, leading to a dysbiosis which will eventually trigger an inflammatory syndrome.”
Interestingly, the infected mice had several signs of debilitating gut inflammation. Endoscopies revealed colons from infected mice had 4.5 times higher levels of particular inflammatory molecules (called IFN-γ) associated with colitis. Under the microscope, infected intestinal tracts also had more severe visual signs of swelling than those from uninfected mice.
“As a next step, we want to confirm the role of the fungi in the pathogenesis of Crohn's disease by treating infected mice with antifungal drugs to decrease symptoms of intestinal inflammation,” Dr. Di Martino noted. “If our hypothesis is right, that would open the door to novel antifungal therapies to treat Crohn's disease patients.”
The authors concluded that “our data demonstrate that C. tropicalis may play a proinflammatory role in intestinal injury by exacerbating gut inflammation during the recovery phase of dextran sodium sulfate-induced colitis. We speculate that infection with the fungus C. tropicalis may play a role in triggering flares during Crohn's disease and that antifungal therapy may be beneficial in Crohn's disease patients.”