The results of research headed by a team at Albert Einstein College of Medicine suggest that revving up a cellular housekeeping process that slows down as we age may protect against atherosclerosis. Ana Maria Cuervo, MD, PhD, and colleagues successfully minimized artery-narrowing plaque in mice that would otherwise develop those lesions, by boosting chaperone-mediated autophagy (CMA), a process that Cuervo discovered in 1993, and gave a name to in 2000.
“We’ve shown in this research that we need CMA to protect against atherosclerosis, which becomes severe and progresses when CMA declines—something that also happens when people get older,” Cuervo, who is professor of developmental and molecular biology and of medicine, the Robert and Renée Belfer chair for the study of neurodegenerative diseases, and co-director of the Institute for Aging Research at Einstein. “But equally important, we’ve proven that increasing CMA activity can be an effective strategy for curbing atherosclerosis and halting its progression.”
Cuervo and colleagues reported on their findings in Proceedings of the National Academy of Sciences, in a paper titled “Protective role of chaperone-mediated autophagy against atherosclerosis,” in which they concluded, “We propose that CMA could be an attractive therapeutic target against cardiovascular diseases.”
Cardiovascular disease (CVD) is the leading underlying cause of death worldwide, accounting for more than 31.5% of total deaths, the authors wrote. “The main risk factors for the development of atherosclerosis—the most common cause of CV clinical events—such as obesity, hypertension, diabetes, and aging are rising in epidemic proportions due to changes in lifestyle and the growing elderly population.”
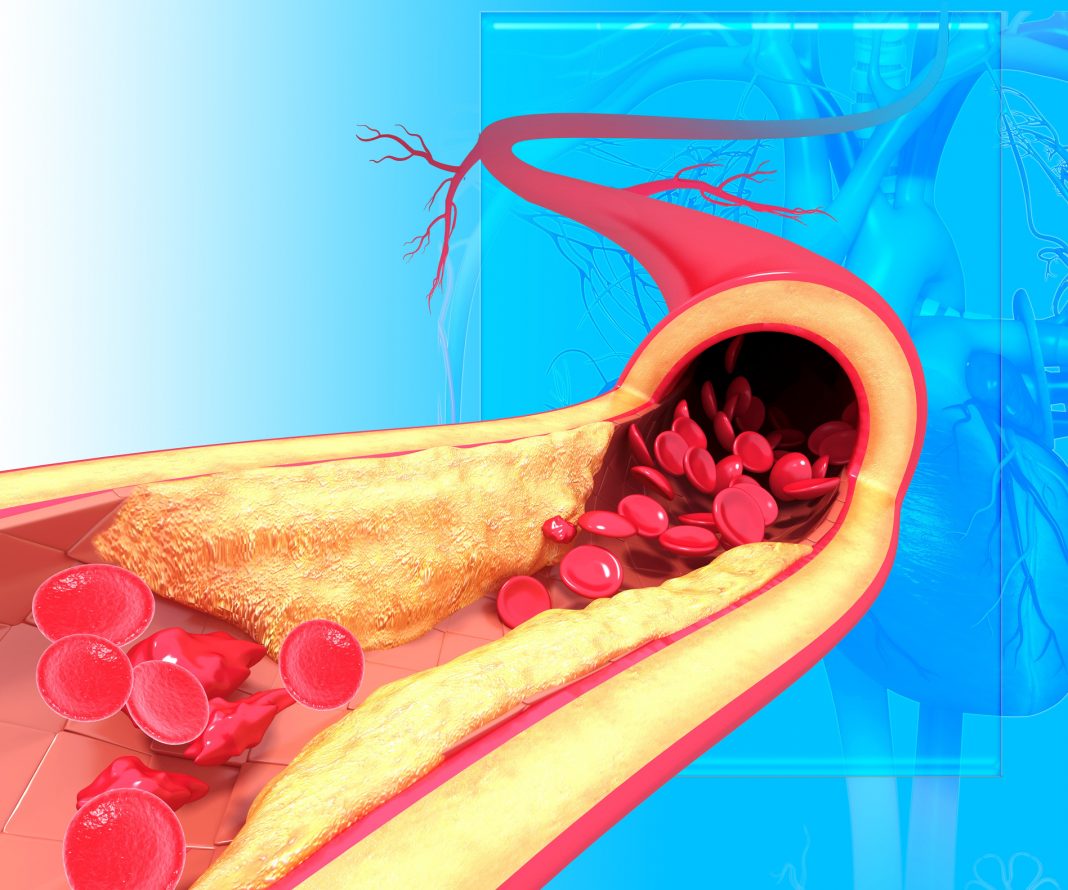
Atherosclerosis is the build up of plaque (a sticky material consisting of fat, cholesterol, calcium, and other substances) within the walls of arteries. Accumulating plaque hardens and narrows arteries, preventing them from delivering oxygenated blood to heart muscle, the brain, and other parts of the body, and potentially leading to heart attack and stroke.
CMA keeps cells functioning normally by selectively degrading the many proteins that cells contain. In CMA, specialized “chaperone” proteins bind to proteins in the cytoplasm and guide them to enzyme-filled lysosomes, to be digested and recycled.
Cuervo’s research has deciphered many of the molecular players involved in CMA and shown that this process regulates numerous intracellular processes including glucose and lipid metabolism, circadian rhythms, and DNA repair. “CMA contributes to regulation of energy homeostasis by timely degradation of enzymes involved in glucose and lipid metabolism,” the authors continued. Cuervo had in addition found that disrupted CMA allows damaged proteins to accumulate to toxic levels, contributing to aging and—when the toxic build up occurs in nerve cells—to neurodegenerative diseases including Parkinson’s, Alzheimer’s, and Huntington’s disease.
Her achievements were recognized in 2019 when she was elected to the National Academy of Sciences. Following COVID-19-related delays, the new report on the protective role of CMA against atherosclerosis is her inaugural PNAS paper, which adds to her body of work on the importance of CMA.
To investigate CMA’s role in atherosclerosis, Cuervo and colleagues promoted atherosclerosis in mice by feeding them a fatty Western diet for 12 weeks, and then monitoring CMA activity in the animals’ plaque-affected aortas. The researchers found that CMA activity initially increased in response to the dietary challenge, but after 12 weeks there was significant plaque build up and virtually no CMA activity could be detected in the two types of cells—macrophages and arterial smooth muscle cells—that are known to malfunction in atherosclerosis, leading to the build up of plaque within arteries. “We have identified that CMA is up-regulated early in response to proatherogenic challenges and demonstrate that reduced systemic CMA aggravates the vascular pathology in these conditions,” they wrote.
Cuervo commented: “CMA seemed to be very important in protecting macrophages and smooth muscle cells—helping them function normally despite the pro-atherosclerotic diet—at least for a while, until their CMA activity basically came to a halt.” She noted that feeding the high-fat diet (HFD) to mice totally lacking in CMA activity produced even stronger evidence of CMA’s importance, and in these animals, plaques were nearly 40% larger than those in control animals that were also on the HFD. “… in vivo genetic blockage of CMA worsens atherosclerotic pathology through both systemic and cell-autonomous changes in vascular smooth muscle cells and macrophages, the two main cell types involved in atherogenesis,” the authors stated. The investigators separately reported evidence that weak CMA activity correlates with atherosclerosis in humans. Some patients who have had strokes undergo a surgical procedure known as carotid endarterectomy to remove plaque-affected segments of their carotid arteries and so reduce the risk of a second stroke.

The team suggests their study is the first to show that turning up CMA could be an effective way to prevent atherosclerosis from becoming severe or progressing. HFD-fed mice that were genetically engineered to upregulate CMA exhibited greatly improved blood lipid profiles, with markedly reduced levels of cholesterol when compared with control mice fed an HFD. Plaque lesions that formed in the genetically altered mice were also significantly smaller and milder in severity compared with plaques in control mice. “We show that genetic activation of CMA slows down disease progression in mice, supporting a potential therapeutic value of CMA up-regulation in atherosclerosis,” the team commented.
In their discussion, the team further commented, “We propose that up-regulation of CMA is part of the organism’s response to proatherogenic challenges, but that factors such as aging or sustained dietary pressure, known to inhibit CMA, reduce the efficacy of this protective mechanism.”
Boosting CMA in humans may be possible pharmacologically, the authors noted. “My colleagues and I have developed drug compounds that have shown promise for safely and effectively increasing CMA activity in most mouse tissues and in human-derived cells,” said Cuervo. Einstein has filed intellectual property on the underlying technology.