Approaching the immune system as though it were a work of engineering in need of improved cancer-fighting programming, MIT scientists have developed gene circuits that alter gene expression in cancer cells, causing the cancer cells to come to the notice of T cells, which respond by killing the cancer cells selectively, sparing healthy cells.
The scientists say that their synthetic biology approach, which has been shown to work in an in vivo model of ovarian cancer, as well as in an animal model, can be tweaked to recognize other cancers. By treating the genomes of different kinds of cells as though they were application platforms, the scientists hope that they will eventually be able to use the immune system to target other diseases such as rheumatoid arthritis, inflammatory bowel disease, and other autoimmune diseases.
The installation of synthetic gene circuits that work only in cancer cells represents a new form of cancer immunotherapy, which has shown considerable potential, but still faces stubborn challenges. Existing approaches to cancer immunotherapy have been demonstrated successfully in several recent clinical trials, according to Timothy Lu, M.D., Ph.D., associate professor of biological engineering and of electrical engineering and computer science at MIT.
“There has been a lot of clinical data recently suggesting that if you can stimulate the immune system in the right way you can get it to recognize cancer,” said Lu, who is head of the Synthetic Biology Group in MIT's Research Laboratory of Electronics. “Some of the best examples of this are what are called checkpoint inhibitors, where essentially cancers put up stop signs [that prevent] T cells from killing them. There are antibodies that have been developed now that basically block those inhibitory signals and allow the immune system to act against the cancers.”
However, despite this success, the use of immunotherapy remains limited by the scarcity of tumor-specific antigens—substances that can trigger an immune system response to a particular type of cancer. The toxicity of some therapies, when delivered as a systemic treatment to the whole body, for example, is another obstacle.
What's more, the treatments are not successful in all cases. Indeed, even in some of the most successful tests, only 30% to 40% of patients will respond to a given therapy, Lu noted.
As a result, there is now a push to develop combination therapies in which different but complementary treatments are used to boost the immune response. So, for example, if one type of immunotherapy is used to knock out an inhibitory signal produced by a cancer, and the tumor responds by upregulating a second signal, an additional therapy could then be used to target this one as well, Lu says.
“Our belief is that there is a need to develop much more specific, targeted immunotherapies that work locally at the tumor site, rather than trying to treat the entire body systemically,” Lu continued. “Secondly, we want to produce multiple immunotherapies from a single package, and therefore be able to stimulate the immune system in multiple different ways.”
To do this, Lu and a team including MIT postdocs Lior Nissim, Ph.D., and Ming-Ru Wu, M.D., Ph.D., have built a gene circuit encoded in DNA designed to distinguish cancer cells from noncancer cells. Lu and colleagues described their work October 19 in Cell, in an article entitled “Synthetic RNA-Based Immunomodulatory Gene Circuits for Cancer Immunotherapy.”
“Our design comprised de novo synthetic cancer-specific promoters and, to enhance specificity, an RNA-based AND [logic] gate that generates combinatorial immunomodulatory outputs only when both promoters are mutually active,” the article’s authors wrote. “These outputs included an immunogenic cell-surface protein, a cytokine, a chemokine, and a checkpoint inhibitor antibody.”
Cancer cells differ from normal cells in the profile of their gene expression. So, the researchers developed synthetic promoters—DNA sequences designed to initiate gene expression, but only in cancer cells.
The circuit is delivered to cells in the affected area of the body using a virus. The synthetic promoters are then designed to bind to certain proteins that are active in tumor cells, causing the promoters to turn on.
“Only when two of these cancer promoters are activated, does the circuit itself switch on,” Lu emphasized. This allows the circuit to target tumors more accurately than existing therapies, as it requires two cancer-specific signals to be present before it will respond.
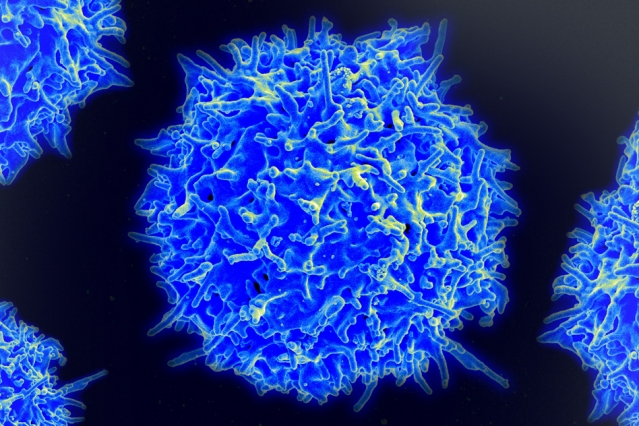
Once activated, the circuit expresses proteins designed to direct the immune system to target the tumor cells, including surface T-cell engagers, which direct T cells to kill the cells. The circuit also expresses a checkpoint inhibitor designed to lift the brakes on T-cell activity.
“The circuits triggered selective T cell-mediated killing of cancer cells, but not of normal cells, in vitro,” the Cell article indicated. “In in vivo efficacy assays, lentiviral circuit delivery mediated significant tumor reduction and prolonged mouse survival.”
When the researchers tested the circuit in vitro, they found that it was able to detect ovarian cancer cells from amongst other noncancerous ovarian cells and other cell types. The researchers then tested the circuit in mice implanted with ovarian cancer cells and demonstrated that it could trigger T cells to seek out and kill the cancer cells without harming other cells around them.
Finally, the researchers showed that the circuit could be readily converted to target other cancer cells.
“We identified other promoters that were selective for breast cancer, and when these were encoded into the circuit, it would target breast cancer cells over other types of cell,” Lu explained.
The researchers now plan to test the circuit more fully in a range of cancer models. They are also aiming to develop a delivery system for the circuit, which would be both flexible and simple to manufacture and use.