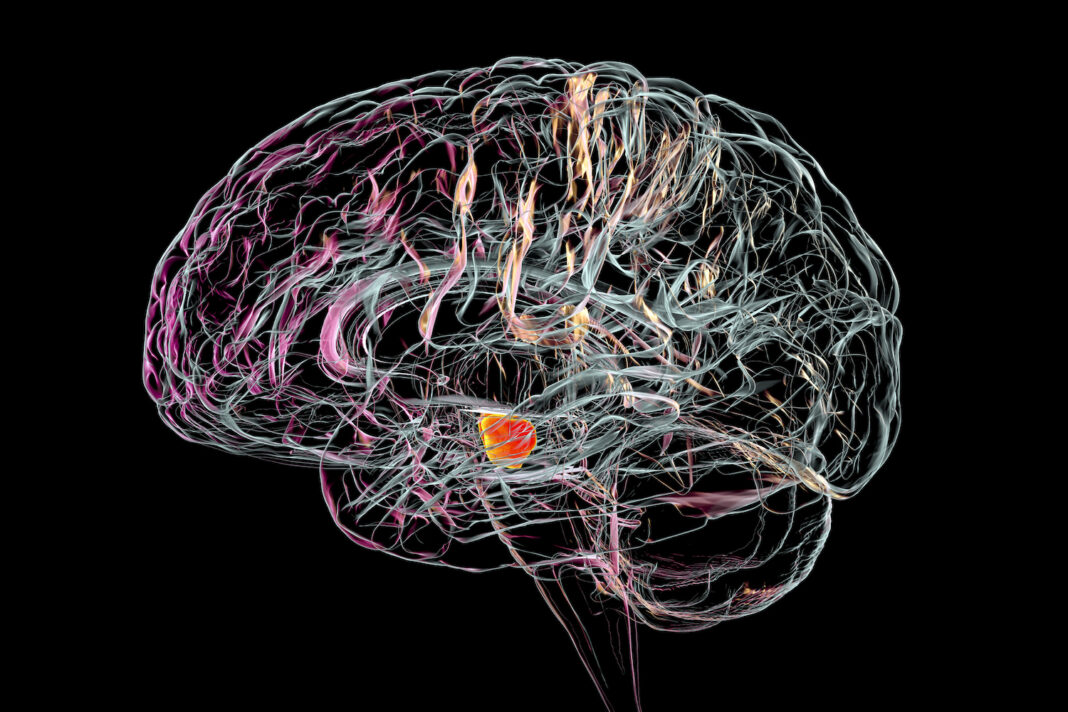
There may be a link between the SARS-CoV-2 infection of dopaminergic neurons and the long-term effects of COVID-19 symptoms like depression and brain fog, according to new research. Dopaminergic neurons derived from human pluripotent stem cells (hPSC) infected with SARS-CoV-2 undergo senescence, marked by inflammation and a decline in function. The researchers went on to show that several FDA-approved medications can stop SARS-CoV-2 infection-induced dopaminergic neuron senescence.
The research article, “SARS-CoV-2 infection causes dopaminergic neuron senescence,” was published in Cell Stem Cell.
COVID-19 and nervous system dysfunction
Patients with COVID-19 often exhibit symptoms of neurological dysfunction. More and more abnormal neurological symptoms in COVID-19 patients are being identified; these symptoms include anosmia, dysgeusia, headache, seizures, stroke, and acute inflammatory polyradiculoneuropathy (Guillain-Barre syndrome) as the most common ones. Additionally, a large retrospective cohort found an increased risk for additional neurological and psychiatric disorders at six months post-diagnosis.
Recent research using organoids made from hPSCs has shown that SARS-CoV-2 can infect cells in the central nervous system that are part of the choroid plexus. Nonetheless, the neuronal tropism of SARS-CoV-2 remains unclear.
Protecting dopaminergic neurons from SARS-CoV-2
A group of researchers from Weill Cornell Medicine, the Sloan-Kettering Institute for Cancer Research, and the Columbia University Vagelos College of Physicians and Surgeons in New York City showed that hPSC-derived dopamine neurons can selectively become infected with SARS-CoV-2. These infected dopaminergic neurons experience a cascade of events culminating in cellular senescence and inflammation.
Low levels of SARS-CoV-2 transcripts and an inflammatory and cellular senescence signature were also found in the human substantia nigra tissue of COVID-19 patients, according to the researchers. Furthermore, they observed reduced functional dopaminergic neurons in a cohort of severe COVID-19 patients.
A high-throughput screen of hPSC-derived dopaminergic neurons showed that several FDA-approved drugs can reverse the cellular senescence phenotype by stopping SARS-CoV-2 infection. The FDA-approved drugs riluzole, metformin, and imatinib were identified to block SARS-CoV-2-mediated dopaminergic neuron senescence.
Both imatinib and metformin have been associated with COVID-19 prevention. Imatinib was previously found to inhibit SARS-CoV-2 entry in a hPSC-derived lung organoid screen. Metformin use has been linked to a lower mortality rate in COVID-19 patients with obesity or type 2 diabetes, and new research suggests that metformin can target dopaminergic neurons. Riluzole, on the other hand, has not previously been linked to SARS-CoV-2 infection. Future research is needed to determine the mechanism of action and translational potential of these compounds and whether they can reverse infection-induced neuropathology.
Previous work indicates that the senescence of dopaminergic neurons can contribute to Parkinson’s disease pathogenesis. As dopaminergic neuron dysfunction is also linked to lethargy and anhedonism, its role in post-COVID-19 lethargy, or “long COVID,” may deserve further study.