University of Leeds scientists have developed a double-barrel nanopipette that allows researchers to see how individual, living cancer cells react to treatment and change over time. This ability could generate vital insights to help doctors develop more effective cancer treatments.
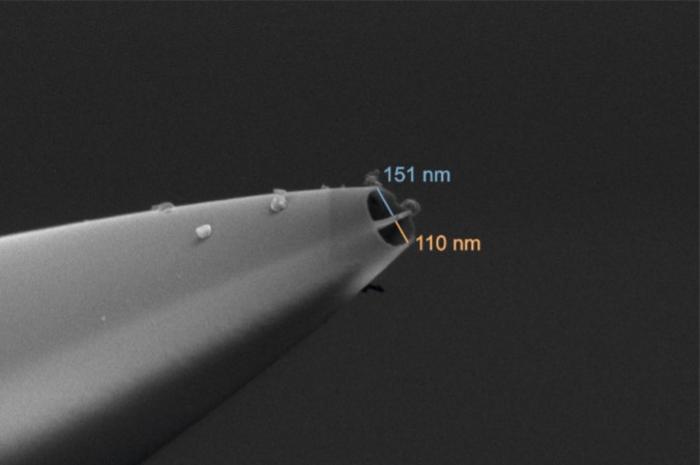
Based on scanning ion conductance microscopy (SICM), the new nanobiopsy platform uses two nanoscopic needles, so it can simultaneously inject into and extract a sample from the same cell. Current techniques for studying single cells usually destroy them, meaning any one cell can be studied either before treatment, or after, but not both. The new device can take a biopsy of a living cell repeatedly during exposure to cancer treatment, sampling tiny extracts of its contents without killing it, enabling scientists to observe transcriptomic changes over time.
The platform also offers high level of semi-automation, making it possible to extract data from many more individual cells, with far greater accuracy and efficiency, than has previously been possible. In their published paper in Science Advances, the multidisciplinary team, including biologists and engineers, reported on their use of the nanopipette platform to biopsy individual glioblastoma (GMB) brain cancer cells and test their resistance to chemotherapy and radiotherapy, over a period of days.
Lucy Stead, PhD, associate professor of Brain Cancer Biology in the University of Leeds’ School of Medicine, said, “This represents a significant breakthrough. It is the first time that we have a technology where we can actually monitor the changes taking place after treatment, rather than just assume them. This type of technology is going to provide a layer of understanding that we have simply never had before. And that new understanding and insight will lead to new weapons in our armory against all types of cancer.”
Stead is co-corresponding author of the team’s published report in Science Advances, which is titled “Single- cell nanobiopsy enables multigenerational longitudinal transcriptomics of cancer cells.” In their paper the team concluded, “We envisage the nanobiopsy will contribute to transforming standard single-cell transcriptomics from a static analysis into a dynamic assay.”
Much research on molecular biology is carried out on populations of cells, giving an average result that ignores the fact that every cell is different. Some cells die during treatment, but others survive. The key to finding a cure is understanding what allows one cell to survive and what is happening to the ones that die. Single-cell RNA sequencing has revolutionized understanding of cell heterogeneity, the authors noted, but routine methods require cell lysis, and so kill the cells “… and fail to probe the dynamic trajectories responsible for cellular state transitions, which can only be inferred.”
The Leeds-headed group has pioneered the use of nanopipettes integrated into SICM to carry out nanobiopsies of living cells in culture. “The nanobiopsy technique has enabled the extraction of RNA and organelles from single cells, the study of mRNA compartmentalization within neuronal cells, and the localized sampling of mitochondria from human tissues,” the authors stated.
![Infographic of double barrel nanopipette, demonstrating how it works. [Image designed by Somersault1824. Credit: University of Leeds]](https://www.genengnews.com/wp-content/uploads/2024/03/low-res-3-300x147.jpeg)
One barrel, filled with an organic solution, is used as an electrochemical syringe to perform cytoplasmic extraction, while the second barrel, filled with an aqueous electrolyte solution, provides what the scientists explain is “… a stable ion current for precise positioning and nanoinjection of exogenous molecules into the cell.” Using this double-barrel nanopipette scientists can extract femtoliter volumes of cytoplasm and simultaneously inject exogenous molecules into individual cells, they noted. “This platform offers several advantages compared to previously established techniques … the platform enables multigenerational longitudinal nanobiopsy of the same cell (and its progeny) to profile gene expression changes over 72 hours.”
The study was carried out as a collaboration between researchers from Leeds’ Bragg Center for Materials Research; Leeds’ School of Electronic and Electrical Engineering; Leeds Institute of Medical Research, and the Earlham Institute, Norwich, who studied single GBM cells over the time course of the experiments.

Cancer cell plasticity— the ability of cells to change their behaviors—is one of the biggest challenges in cancer treatment as it remains poorly understood. GBM cancer cells are particularly plastic. They can adapt very quickly, and this is thought to help them develop resistance to radiotherapy and chemotherapy. “The transition of cells between different states confers plasticity to the tumor and it is believed to be responsible for cellular adaptation through therapy,” the investigators wrote. Learning how these cells adapt, and potentially how to then block them from adapting, could prevent cancer from recurring.
Stead added, “GBM is the cancer in most need of those new weapons because in 20 years there has been no improvement in survival in this disease. It is lagging behind so much and we think that is because of the highly ‘plastic’ nature of these tumors—their ability to adapt to treatment and survive it. That is why it is so important that we can dynamically observe and characterize these cells as they change, so we can map out the journey these cells can take, and subsequently find ways to stop them at every turn. We simply couldn’t do that with the technologies that we had.”
Existing single-cell studies haven’t been able to determine whether this shift in GBM cell phenotype after anticancer therapy is due to changes related to cell division and death rates across different cell types, to changes in the phenotype of cell progeny, or is due to direct switching from one cell phenotype to another, the investigators pointed out. In contrast, they stated, “Our technology allowed for the sampling of the same cell and its progeny longitudinally, through therapy, and enabled the determination of phenotype changes that may underpin the ability of these cells to adapt and resist treatment.”
Stead leads the Glioma Genomics research group at the Leeds Institute of Medical Research at St James’s Hospital, which is focused on trying to cure GBM brain tumours. She suggested, “This technology could be transformative for this particular cancer, helping us finally identify effective treatments for this awful, incurable disease.”
The research was primarily funded by The Brain Tumor Charity. The organization’s CSO, Simon Newman, PhD, said, “We know glioblastoma cells respond differently to treatment, often developing treatment resistance which leads to recurrence. The development of this novel technology, which can extract samples from tumour cells grown in the lab before and after treatment, will give a unique insight into how drug resistance may develop and lead to tumors growing back. “We hope that this important work, funded by The Brain Tumor Charity, will improve our knowledge of these complex brain tumours and allow us to find new, more effective treatments—something so urgently needed for those faced with this devastating disease.”
Lead study author Fabio Marcuccio, PhD, research associate in the Faculty of Medicine at Imperial College London, who carried out the research while at Leeds, further noted, “Our device allows the study of the way brain cancer cells adapt to treatment over time, with unprecedented precision. This tool will provide data that could lead to significant improvements in cancer treatment and prognoses.”
He added: “This work is the result of a collaborative effort with my colleagues and co-leads Chalmers Chau, PhD, research fellow in Bionanotechnology in Leeds’ School of Electronic and Electrical Engineering, and Georgette Tanner, PhD, formerly of Leeds, now Bioinformatician at Oxford Nanopore Technologies, whose contributions were fundamental to the experimental design and data analysis. This demonstrates the importance of creating an interdisciplinary team to tackle the biggest challenges of our time.”
Study co-lead and co-corresponding author, Paolo Actis, PhD, associate professor of Bio-Nanotechnology in Leeds’ School of Electronic and Electrical Engineering, has been working on the nanobiopsy tool for around 15 years and said its new capabilities, compared to its original scope, provided “remarkable advantages”. He added, “Cancer cells that are not killed by chemotherapy are the ones that make the cancer grow back and lead to death. Our tool can pinpoint these cells and we can now perform biopsies on them so we can specifically study how the ones that survive treatment have changed. This is crucially important as the more we can understand how the cells change, the more drugs we can develop to stop them from adapting.”
Stead said further research needed to be carried out, using this technology on many more samples in the lab and in humans, but that it had already yielded hugely valuable information.