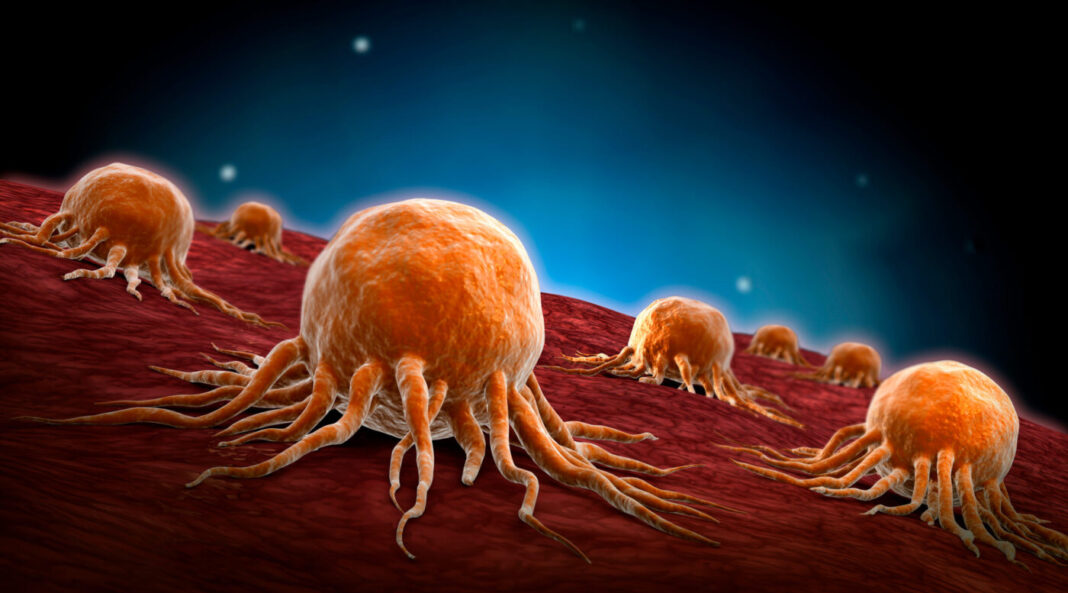
Many cancers are not inflamed and thus, are not recognized by the immune system. Since these “cold” tumors do not elicit a response from the immune system, they do not respond to immunotherapies. “Hot” tumors show signs of inflammation, which means they can be infiltrated with T cells working to fight the cancer. These tumors are easier to treat, as immunotherapy drugs can boost up the immune response.
Using mouse models, researchers from the University of Colorado Cancer Center have discovered that regulatory T cells (Tregs), a specialized T cell type that suppresses immune response, are essentially telling the T cells to stop fighting the cancer. Their findings present a new therapeutic opportunity for treating cold tumors and head and neck squamous cell carcinomas (HNSCC) that are resistant to radiation therapy.
The study is published in the Journal for ImmunoTherapy of Cancer in a paper titled, “Targeting resistance to radiation-immunotherapy in cold HNSCCs by modulating the Treg-dendritic cell axis.”
“Numerous trials combining radiation therapy (RT) and immunotherapy in HNSCC are failing,” wrote the researchers. “Using preclinical immune cold models of HNSCC resistant to RT-immune checkpoint inhibitors, we investigated therapeutic approaches of overcoming such resistance by examining the differential microenvironmental response to RT.”
The team was led by Michael Knitz, research assistant, and Sana Karam, MD, PhD, associate professor of radiation oncology at the University of Colorado School of Medicine and University of Colorado Cancer Center member. Using mouse models, the researchers studied the role of T cells in tumor treatment.
“What we found is that the cells that normally tell the T cell, ‘Hey, here’s a tumor—come and attack it,’ are being silenced,” Karam said.
“Tregs normally serve as an important balance in a healthy immune system,” Knitz said. “They prevent autoimmune disease and put the brakes on the T cells when needed. However, in many tumors, Tregs are too numerous or overly suppressive, bringing the T cell response to a halt.”
The researchers discovered that using medication that deactivates the Tregs can help boost the immune response in patients with cold tumors. The researchers also noted that radiation treatment causes enough injury that dendritic cells can work to put the regular T cells into fight mode.
“You need the radiation to create injury and bring in the immune cells so that the tumor can be recognized and targeted,” explained Karam. “That way, the dendritic cells trigger the immune system to produce a lot of T cells, similar to what a vaccine does. Those T cells then go back to the tumor to kill cancer cells. The pieces are already in place; they just need the proper signals. Activating the dendritic cells is a crucial step in allowing radiation to heat up these cold tumors.”
The researchers noted that the radiation must be administered in a specific way. “You have to pulse it. You can’t just give one dose. You have to give it again and combine it with things that remove the suppression—the Tregs—while simultaneously keeping those antigen-presenting dendritic cells active and on board.”
Karam is driven to change the standard of care for cold tumors. “These tumors resemble those in patients who are heavy smokers,” she stated. “They’re very destructive to bone and muscle, infiltrating the tongue, jaw, gum, and lymph nodes. It’s horrible. We have very high failure rates with them, and the treatment often involves removing the tongue and weeks of radiation and chemotherapy, only for the patient to fail. I’m confident that we can do better for our patients.”