A new study by researchers at the University of California (UC) San Diego uncovers insights into the biology of tissue-specific T cells. Their study reveals the complexity of tissue-resident memory (TRM) cell biology in the gut, which may lead to a new generation of precision therapeutics against infection, cancer, and auto-immune disease.
The findings are published in the journal Immunity in an article titled, “Small intestine and colon tissue-resident memory CD8+ T cells exhibit molecular heterogeneity and differential dependence on Eomes.”
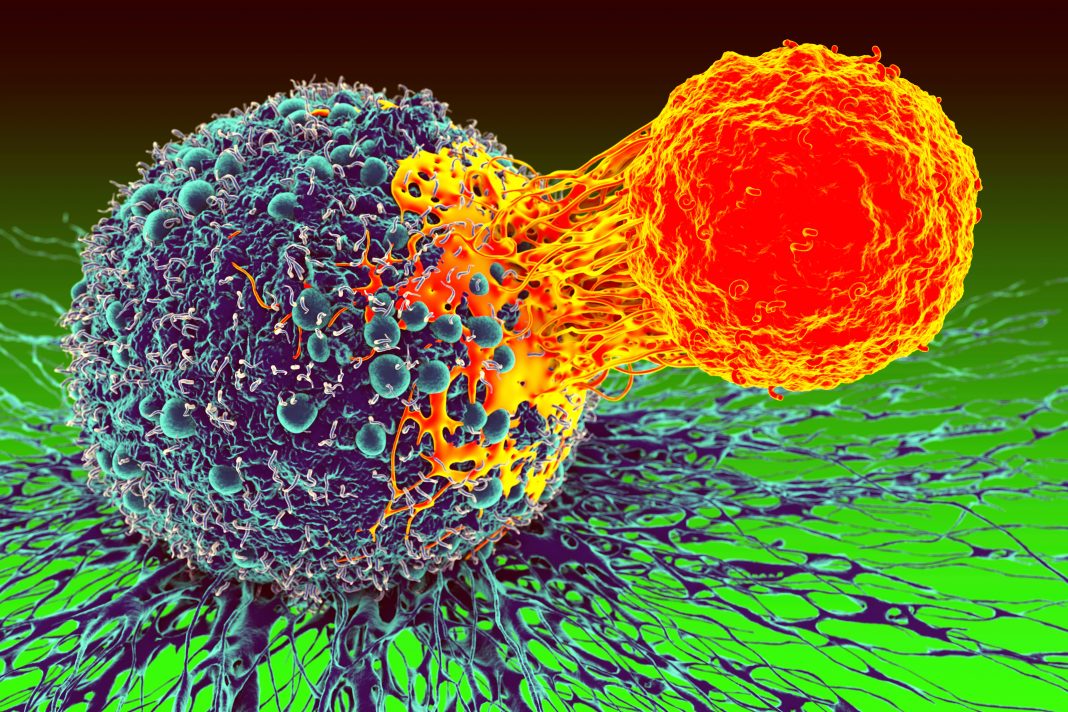
“Tissue-resident memory CD8+ T cells are a subset of memory T cells that play a critical role in limiting early pathogen spread and controlling infection,” wrote the researchers. “TRM cells exhibit differences across tissues, but their potential heterogeneity among distinct anatomic compartments within the small intestine and colon has not been well recognized. Here, by analyzing TRM cells from the lamina propria and epithelial compartments of the small intestine and colon, we showed that intestinal TRM cells exhibited distinctive patterns of cytokine and granzyme expression along with substantial transcriptional, epigenetic, and functional heterogeneity.”
“TRM cells are the first responders, right at the front lines of infection,” said senior author John T. Chang, MD, professor at UC San Diego School of Medicine. “Most of our vaccines are designed to provide systemic immunity, but we may be able to get even better protection by instead focusing on boosting the tissue-specific cells that encounter the pathogen first.”
The researchers performed a series of experiments to characterize TRM cells in mice from four different compartments of the gut: the small intestine and the colon, and the intraepithelial and lamina propria layers.
The researchers observed that TRM cells in each tissue type exhibited distinct patterns of cytokine and granzyme expression, along with substantial transcriptional, epigenetic, and functional heterogeneity. The same type of immune cells in each part of the gut appeared to be very different in their molecular makeup, function, and chemical signals they depend on.
Each population of cells also showed differential dependence on Eomesodermin (Eomes), a transcriptional factor known to affect TRM cell development.
The researchers look forward to researching the rules of TRM cell formation and maintenance in other tissues and exploring what drives their specificity.
“In the future, we want to be thinking about vaccines and other therapeutics that are tailored to the specific needs of each organ,” said Chang. “By knowing what each tissue type needs to support the formation and maintenance of TRM cells, we can provide the most efficient immune defenses against disease.”