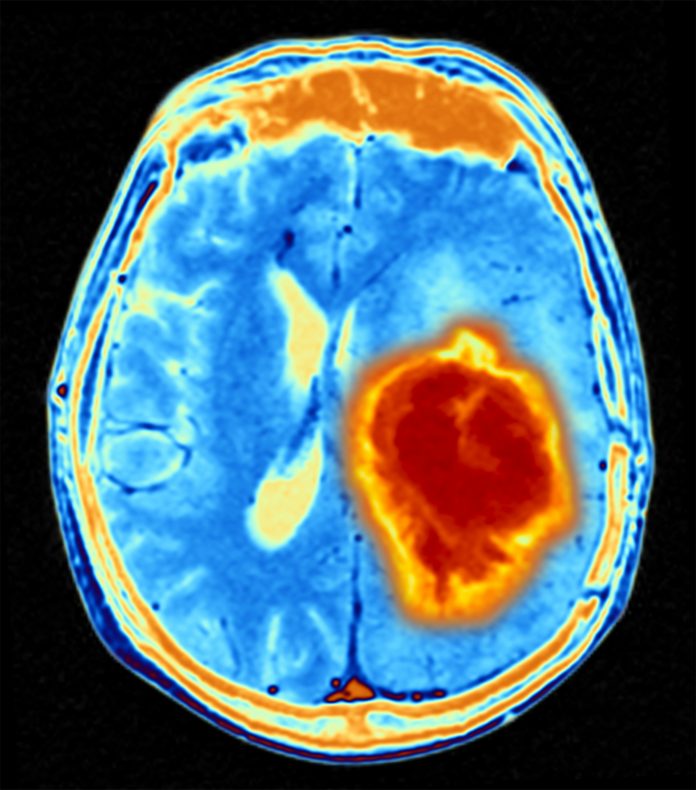
Cancer cells release “don’t eat me” signals to evade immune attack. Immunotherapy attempts to enable these cells to eradicate the abnormal cells, but so far, it has had little success when it comes to battling against glioblastomas. Now, researchers led by Professor Gregor Hutter from the department of biomedicine at the University of Basel and the University Hospital Basel have recently used patient data, experiments with mice, and samples from human tumors to study one of the “don’t eat me!” signals and its inhibitory effect.
Their findings are published in Science Translational Medicine in an article titled “Targeting the Siglec–sialic acid axis promotes antitumor immune responses in preclinical models of glioblastoma.”
“Glioblastoma (GBM) is the most aggressive form of primary brain tumor, for which effective therapies are urgently needed,” wrote the researchers. “Cancer cells are capable of evading clearance by phagocytes such as microglia- and monocyte-derived cells through engaging tolerogenic programs. Here, we found that high expression of sialic acid–binding immunoglobulin-like lectin 9 (Siglec-9) correlates with reduced survival in patients with GBM. Using microglia- and monocyte-derived cell-specific knockouts of Siglec-E, the murine functional homolog of Siglec-9, together with single-cell RNA sequencing, we demonstrated that Siglec-E inhibits phagocytosis by these cells, thereby promoting immune evasion.”
The signal is based on sugar molecules called sialic acid glycans on the surface of the cancer cells. These sugar molecules are recognized by “receivers” on the surface of the brain’s macrophages and interpreted as “don’t eat me!” Hutter’s team of researchers reports that patients whose macrophages have especially high numbers of these “Siglec9” receivers have a lower survival rate.
When the researchers used a genetic trick to remove the mouse variant of Siglec9 from the brain macrophages of laboratory mice, brain tumors in these mice grew significantly more slowly. The researchers observed the macrophages no longer had the receiver that allowed them to perceive the “don’t eat me!” signal, so they were able to proceed with their task of removing the abnormal cells.
The researchers confirmed this in experiments with surgically-removed brain tissue from glioblastoma patients, which the researchers cultivated in the lab.
“Taken together, our results suggest that the sialic acid-Siglec axis could be a promising therapeutic target,” Hutter explained.
The next step in the team’s research is to examine in clinical studies whether it is possible to provide a local dose of antibodies against the receiver in the brain and whether this has the desired effect.