Cancer drugs have an extremely high rate of clinical trial failure. The majority of them do not succeed in advancing to clinical use because of problems with efficacy or toxicity—often for unclear reasons. Jason Sheltzer, PhD, research fellow at Cold Spring Harbor Labs (CSHL) hypothesized that this may be due to problems with the design and development of cancer drugs.
His team led research revealing that a drug candidate in clinical development was effective at killing cancer cells even when its target protein was knocked out, suggesting that its proposed mechanism of action was incorrect. They went on to identify 10 cancer drugs, based on RNAi, that are currently in clinical trials that do not work how clinicians thought they would.
Their work is published in Science Translational Medicine in a paper titled, “Off-target toxicity is a common mechanism of action of cancer drugs undergoing clinical trials“.
Previous work in the Sheltzer lab identified genes tied to low survival rates among cancer patients. In doing so, they discovered that MELK, a protein often found in high levels in tumors, has absolutely no influence on cancer growth despite MELK having been identified as a cancer “addiction”—something absolutely essential for a cancer cell’s survival. Yet, when Sheltzer and his lab directly turned off MELK production using CRISPR, affected cancer cells were unphased.
“To our great surprise, the cancer cells didn’t die,” Sheltzer reported last year. “They just didn’t care about MELK.” After rigorously checking and rechecking their results, Sheltzer’s lab had to conclude that MELK is not the ideal cancer drug target it was touted to be.
At the time, Sheltzer and his colleagues warned research and medical communities that this may be a common problem, leading to any number of promising cancer drugs being mischaracterized.
“The idea for many of these drugs is that they block the function of a certain protein in cancer cells. And what we showed is that most of these drugs don’t work by blocking the function of the protein that they were reported to block,” Sheltzer explained.
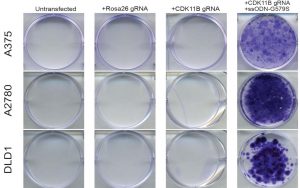
Using CRISPR-Cas9 mutagenesis, the team investigated a set of cancer drugs and drug targets in various stages of clinical testing. All 10 of the tested drugs do appear capable of killing cancer cells—it’s just not in the way researchers had thought.
“In some sense, this is a story of this generation’s technology,” Sheltzer said. RNA interference (RNAi) allowed researchers to prevent the instructions for producing a protein made by any one gene to be read by a cell. But, there is also the chance that the process will covertly interfere with the production of one of the thousands of other proteins found in a human cell.
That’s what Sheltzer and his colleagues suspected was happening not only with MELK but with the six other promising proteins targeted by those 10 experimental cancer drugs. Something was also being affected, and it was this off-target effect that was truly stopping cancer. Using the more accurate CRISPR technology, this was what his team set out to discover.
To do this, they took one of the 10 drugs—in this case, one which kills cancer cells by supposedly inhibiting the protein PBK. But Sheltzer found it was doing something very different. “It turns out that this interaction with PBK has nothing to do with how it actually kills cancer cells,” Sheltzer said.
To find out the true anticancer mechanism of action, his team exposed cancer cells to “a very, very high concentration” of the PBK-targeting drug. The researchers then gave the cells plenty of time to develop a drug resistance.
“Cancers are highly genomically unstable. Because of this inherent instability, every cancer cell in a dish is different from the one next to it. A cancer cell which randomly acquires a genetic change that blocks the effectiveness of a drug will succeed where the others are killed,” Sheltzer explained. “We can take advantage of this. By identifying that genetic change, we also can identify how the drug was killing cancer.”
The team found that the cancer cells evolved their resistance by mutating the gene that produces the protein CDK11 in such a way that the drug can no longer interact with it. Along with some other confirmatory experiments, this told the team that CDK11 is the true mechanism of action against cancer. Armed with this knowledge, the researchers now hope to design even better drugs that target CDK11 more specifically.
“A lot of drugs that get tested in human cancer patients tragically don’t end up helping cancer patients,” Sheltzer said. “If this kind of evidence was routinely collected before drugs entered clinical trials, we might be able to do a better job assigning patients to therapies that are most likely to provide some benefit. With this knowledge, I believe we can better fulfill the promise of precision medicine.”


