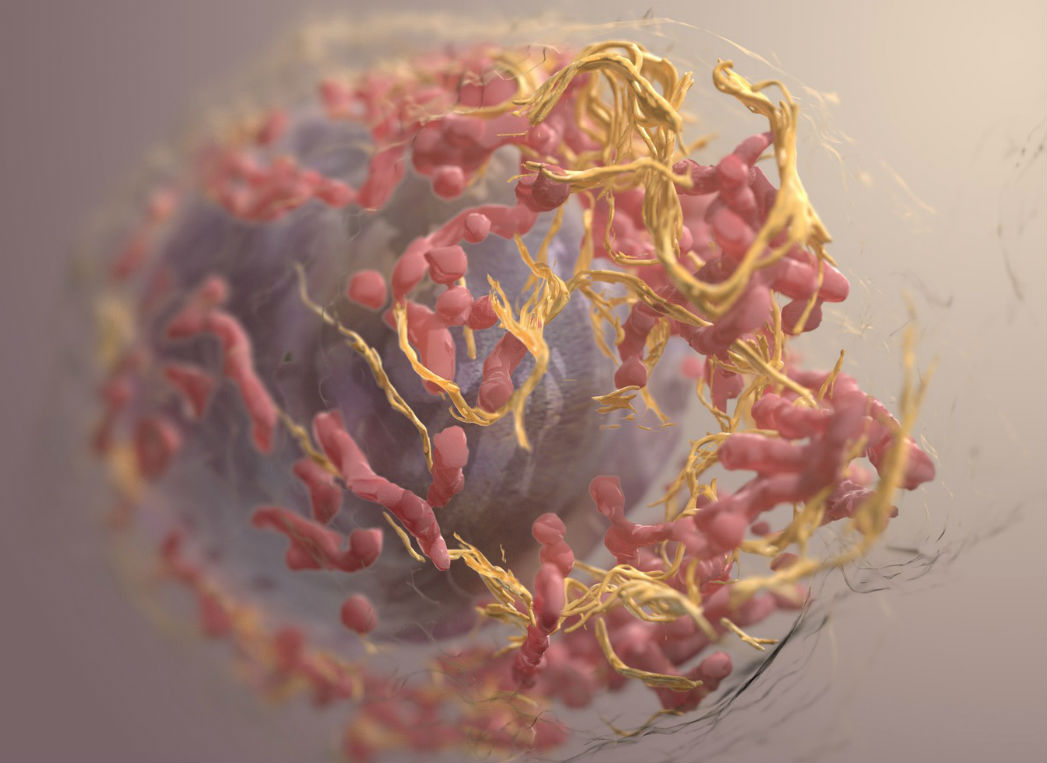
Programmed cell death protein 1 (PD-1) and CTLA-4 (cytotoxic T-lymphocyte-associated protein 4) are proteins found on the surface of immune cells that downregulate immune response. The inhibition of these proteins—dual immune checkpoint therapy–constitutes the most effective approach for activation of anti-tumor immune responses in the treatment of many types of cancers.
Although combined PD-1 and CTL-4 therapy improves overall survival in various cancers it is also accompanied by immune-related adverse events, such as colitis, an inflammatory bowel disease.
Reliable biomarkers that would help clinicians distinguish between patients who are most likely to respond favorably to combined checkpoint inhibitors and patients who are most likely to develop severe toxicity to the treatment are currently lacking.
A new study led by researchers from the University of Texas MD Anderson Cancer Center reports intestinal microbiota signatures correlate with high-grade adverse events in response to combined CTLA-4 and PD-1 blockade treatment. The scientists identify a potential new strategy to treat toxicity while maintaining response to combined immune checkpoint blockade through either IL-1R inhibition or manipulation of gut microbiota.
The study published in the Nature Medicine article, “Gut microbiota signatures are associated with toxicity to combined CTLA-4 and PD-1 blockade,” was financially supported by multiple agencies including Région Provence Alpes Côte d’Azur, European funding FEDER PRIMI and philanthropic contributions from the Lyda Hill Foundation, Dr. Miriam and Sheldon G. Adelson Medical Research Foundation and the AIM at Melanoma Foundation.

“This study further highlights the importance of the gut microbiome in both response as well as in toxicity in patients being treated with combined immune checkpoint blockade,” says Jennifer Wargo, MD, professor of Genomic Medicine and Surgical Oncology and senior author on the study. “We’re committed to understanding and addressing the significant immune-related side effects that tend to accompany this combination therapy, so that patients don’t have to compromise quality of life for effective cancer treatment.”
The study was conducted on 77 adult patients who received combined CTLA-4 and PD-1 blockade treatment for advanced melanoma at MD Anderson. The majority had stage IV disease and had not received any previous systemic therapy. Nearly all patients had an adverse event of any grade and about half experienced grade 3 or higher adverse events in response to treatment.
The authors found patients with advanced melanoma who experienced toxicity from combined immunotherapy had considerably higher numbers of the gut microbe Bacteroides intestinalis. They confirm a high levels of B. intestinalis in the gut is associated with increased mucosal interlukin-1β and inflammation in preclinical animal models and patients.
Toward finding a way to reduce toxicity while maintaining response to combined immune checkpoint blockade, the team uses a drug (anakinra) approved for the treatment of rheumatoid arthritis to inhibit interleukin-1 receptor and successfully reduce intestinal inflammation without blunting the efficacy of the immune therapy in preclinical models.
The scientists also show patients who experienced grade 3 or higher adverse events had a more diverse T cell repertoire and a more naïve T cell phenotype in the systemic circulation. Whole-exome sequencing shows higher tumor mutational burden in responders, compared to non-responders. Non-responders show a higher level of copy number loss, mostly in chromosomes 5, 10 and 15.
These findings corroborate earlier studies that suggest tumor mutational burden is associated with response and copy number loss is associated with resistance. Tumor biopsies at baseline reveal a higher density of CD8+ T cells in responders, compared to non-responders.
“We’re getting closer to understanding which patients are most likely to benefit from checkpoint inhibitors and to identifying strategies to mitigate toxicity,” says Wargo. “We’re grateful to the patients who have participated in our ongoing research; they continue to motivate and inspire us as we undertake additional studies to build upon the insights from this research.”
Larger cohort studies will be needed to validate the biomarkers for toxicity and response and to investigate IL-1R inhibition as a potential therapeutic target for inflammation.