Researchers at Columbia University have developed a probiotic-guided chimeric antigen receptor (CAR)-T platform that uses engineered bacteria to infiltrate and produce synthetic antigen targets, enabling CAR-T cells to find, identify, and destroy tumor cells in situ. The results of in vivo preclinical tests suggest that the combined ProCAR cell therapy platform could expand the scope of CAR-T cell therapy to include difficult-to-target solid tumors.
Tal Danino, PhD, and Rosa L. Vincent, PhD, at Columbia University’s department of biomedical engineering, and colleagues, reported on their developments in Science, in a paper titled “Probiotic-guided CAR-T cells for solid tumor targeting,” in which they concluded, “These findings highlight the potential of the ProCAR platform to address the roadblock of identifying suitable CAR targets by providing an antigen that is orthogonal to both healthy tissue and tumor genetics … Overall, combining the advantages of tumor-homing bacteria and CAR-T cells provides a new strategy for tumor recognition and, in turn, builds the foundation for engineered communities of living therapies.”
Immunotherapies using CAR-T cells have proven successful in treating some types of blood cancers, but their efficacy against solid tumors remains elusive. A key challenge facing tumor-antigen targeting immunotherapies like CAR-T is the identification of suitable targets that are specifically and uniformly expressed on solid tumors, the authors noted. “A key challenge of antigen-targeted cell therapies relates to the expression patterns of the antigen itself, which makes the identification of optimal targets for solid tumor cell therapies an obstacle for the development of new CARs.” Solid tumors express heterogeneous and nonspecific antigens and are poorly infiltrated by T cells. As a result, the approach carries a high risk of fatal on-target, off-tumor toxicity, wherein CAR-T cells attack the targeted antigen on healthy vital tissues with potentially fatal effects. “Few tumor-associated antigens (TAAs) identified on solid tumors are tumor restricted, and thus, they carry a high risk of fatal on-target, off-tumor toxicity because of cross-reactivity against proteins found in vital tissues,” the team continued.
Previous studies have shown that, unlike CAR-T cells, which require “considerable engineering to target and infiltrate solid tumors,” some species of bacteria can selectively colonize and preferentially grow within the hostile tumor microenvironments (TMEs) of immune-privileged tumor cores, and can be engineered as antigen-independent platforms for therapeutic delivery.
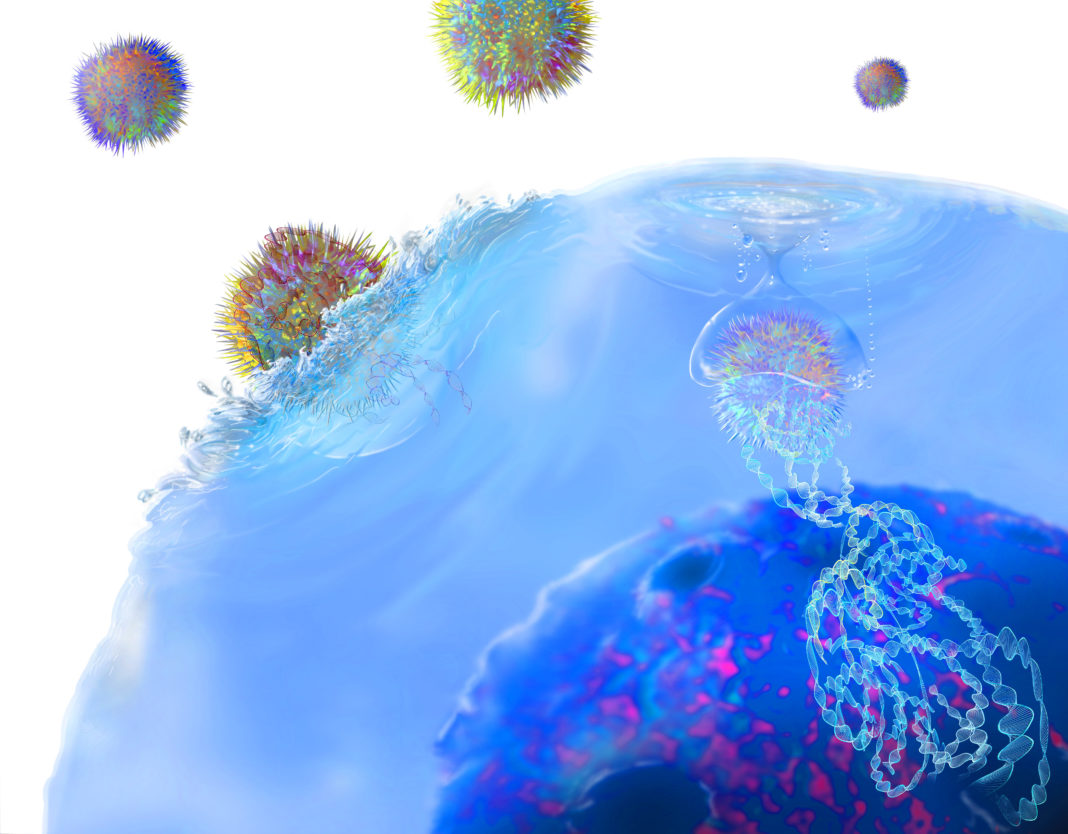
In this study, Vincent, Candice Gurbatri, and colleagues combine probiotic therapy with CAR-T cell therapy to create a two-stage probiotic-guided CAR-T cell (ProCAR) platform, whereby T cells are engineered to sense and respond to synthetic CAR targets that are delivered by solid tumor-colonizing probiotic bacteria. “This approach leverages the antigen independence of tumor-seeking microbes to create a combined cell therapy platform that broadens the scope of CAR-T cell therapy to include difficult-to-target tumors,” the investigators explained.
Using synthetic gene circuit engineering on a well-characterized non-pathogenic strain of E. coli, Vincent et al. created a probiotic that could infiltrate and cyclically release synthetic CAR targets directly to the tumor core, effectively “tagging” the tumor tissue. “With this system, bacterial growth reaches a critical population density exclusively within the niche of the solid TME and subsequently triggers lysis events that cyclically release genetically encoded payloads in situ,” they further explained.
Then, CAR-T cells that were programmed to recognize the probiotic-delivered synthetic antigen tags could be generated that homed in on the tagged solid tumors, killing the tumor cells in situ. The scientists also engineered probiotics that co-released chemokines in addition to synthetic targets to further enhance CAR-T cell recruitment to the tumor, further boosting therapeutic response.
Vincent et al. tested the resulting probiotic-guided CAR-T cell platform in humanized and immunocompetent mouse models of leukemia, colorectal cancer, and breast cancer and showed that it resulted in the safe reduction of tumor volume. “Collectively, these mouse model data demonstrate the use of engineered probiotics to selectively grow within the TME niche and safely release combinations of CAR-T cell enhancing payloads in situ,” they wrote. The team acknowledged that further development of the system will be needed before it can be considered for clinical application. Nevertheless, they stated, “We have demonstrated an approach to engineering interactions between living therapies, in which tumor-colonizing probiotics have been repurposed to guide the cytotoxicity of engineered T cells.”
In a related Perspective, Eric Bressler, PhD, and Wilson Wong, PhD, at Boston University Biomedical Engineering and Biological Design Center, also noted, “Translation of the ProCAR system to the clinic will depend on scalability to larger tumors and attenuation of bacterial strains for safety.” However, they concluded, “The study of Vincent et al. is an important proof-of-concept for a potential approach to treating heterogeneous, immunologically cold, and poorly infiltrated solid tumors.”