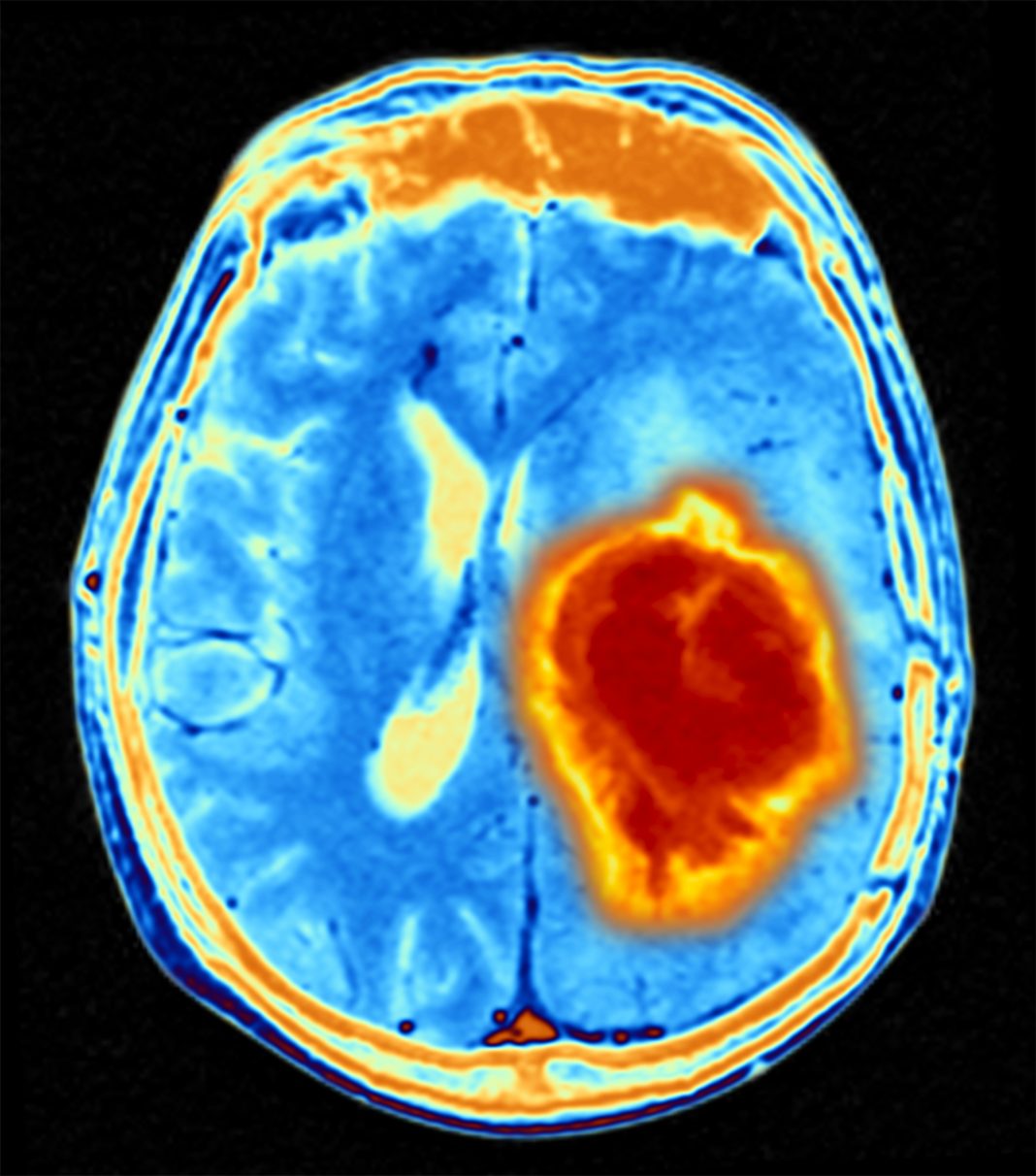
Cerebrospinal fluid is a watery liquid that continually circulates through the brain’s ventricles and around the surface of the brain and spinal cord. It acts like a cushion that helps protect the brain and spinal cord from sudden impact or injury. The fluid also removes waste products from the brain and helps the central nervous system work properly. Now, a new study by researchers at South Australia Health and Medical Research Institute (SAHMRI) and Flinders University demonstrates that cerebrospinal fluid reduces current treatment efficacy in brain cancer and identifies new therapeutic opportunities.
The findings are published in Science Advances in an article titled, “Human cerebrospinal fluid affects chemoradiotherapy sensitivities in tumor cells from patients with glioblastoma.”
“Cancers in the central nervous system resist therapies effective in other cancers, possibly due to the unique biochemistry of the human brain microenvironment composed of cerebrospinal fluid (CSF),” the researchers wrote. “However, the impact of CSF on cancer cells and therapeutic efficacy is unknown. Here, we examined the effect of human CSF on glioblastoma (GBM) tumors from 25 patients. We found that CSF induces tumor cell plasticity and resistance to standard GBM treatments (temozolomide and irradiation).”
The collaborative Australian team of neurobiologists, neurosurgeons, and oncologists tested the effect of the human cerebrospinal fluid on the growth of tumor cells collected from 25 local patients with glioblastoma.
The researchers observed the tumor cells quickly changed their identity and became more resistant to radiation and the drug temozolomide, which are mainstays of glioblastoma therapy.
“Glioblastoma kills so many people who are otherwise fit, healthy, and young, within months,” said Cedric Bardy, PhD, associate professor at Flinders University. “This is a horrible disease, and the treatments available are just not effective enough despite serious side effects. This study helps us understand the limitations of the current chemotherapies and provides new hope for repurposing a class of drugs that could be added to the standard of care. We are working hard now to try this on patients in a clinical trial.”
The team found glioblastoma cells exposed to cerebrospinal fluid were more resistant to ferroptosis, a form of therapy-induced cell death. The researchers noted their study demonstrates the need to diversify the microenvironments used in preclinical screens.
“Altering the patients’ CSF composition for therapeutic goals will be technically difficult or unethical,” noted the researchers. “However, identifying chemotherapies that may prevent CSF-induced cell plasticity or kill CSF-induced cell types, such as TFP or other ferroptosis modulators, provides a more realistic translational solution.”
The researchers identified NUPR1 as one of potential mediators of GBM cell resistance. They also showed that trifluoperazine, an anti-anxiety drug used since the 1950s, is a readily translatable repurposed drug inhibitor of NUPR1, that could re-sensitize glioblastoma cells to both therapies. In contrast, trifluoperazine was found not to harm healthy brain cells. The researchers concluded that combining trifluoperazine with standard care may improve GBM patient survival.