Using a unique stiffness-changing hydrogel system, investigators at the University of California San Diego (UCSD) have uncovered new insights into how the stiffening of breast tissue plays a role in breast cancer development. Findings from the new study—published recently in PNAS through an article titled “Dynamically stiffened matrix promotes malignant transformation of mammary epithelial cells via collective mechanical signaling”—showed that several pathways work together to promote the transformation of breast cells into cancer cells. The researchers are optimistic that their discovery could inspire new approaches to treating patients and inhibiting tumor growth.
“By dynamically modulating the stiffness of the microenvironment, we can better mimic what happens during the transformation of breast cells to a malignant state in a dish,” explained senior study investigator Adam Engler, PhD, a professor of bioengineering at the UCSD Jacobs School of Engineering.
This new study is part of a growing body of research showing that mechanical forces—not just genetic and biochemical signals—play a key role in the development and spread of cancer. In the past, researchers have found that modeling stiff tissue environments in vitro promoted tumor growth. But these models often do not fully recreate what’s happening in the body because they are static, Engler noted.
“Tissue stiffening is a dynamic process. Mammary tissue doesn’t just start out stiff, this is something that develops over time,” Engler noted.
The research team’s approach was to use a material system in which the stiffness could be tuned dynamically while cells are inside, and then see how the cells respond to that change in stiffness.
The UCSD team used a hydrogel called methacrylated hyaluronic acid, a soft material that can be stiffened to varying degrees with exposure to free radicals and UV light. They first stiffened the hydrogel enough to mimic the stiffness of normal breast tissue. Then, they cultured mammary epithelial cells (MECs) in the gel. After the cells matured, the gel’s stiffness was increased to that of a breast tumor. The amount of UV exposure required in this step was not enough to harm the cells, the team noted.
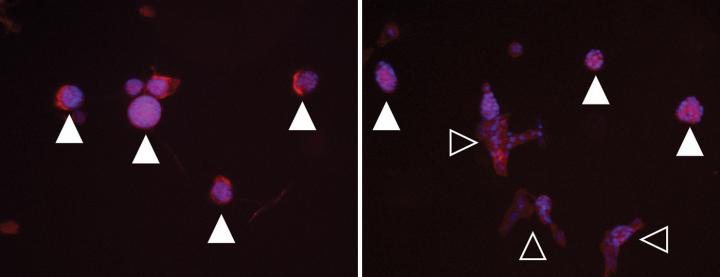
“To more accurately mimic the onset of gradual matrix stiffening, which is not feasible with conventional static hydrogels, MECs were cultured on methacrylated hyaluronic acid hydrogels whose stiffness can be dynamically modulated from ‘normal’ (<150 Pascals) to ‘malignant’ (>3,000 Pascals) via two-stage polymerization,” the authors wrote. “MECs form and remain as spheroids but begin to lose epithelial characteristics and gain mesenchymal morphology upon matrix stiffening. However, both the degree of matrix stiffening and culture time before stiffening play important roles in regulating this conversion as, in both cases, a subset of mammary spheroids remained insensitive to local matrix stiffness. This conversion depended neither on colony size nor cell density, and MECs did not exhibit ‘memory’ of a prior niche when serially cultured through cycles of compliant and stiff matrices.”
Interestingly, the team discovered that stiffening triggers multiple pathways that together signal mammary cells to become cancerous. Key players of these pathways include the proteins TWIST1, TGF-beta, SMAD, and YAP.
“The transcription factor Twist1, transforming growth factor β (TGFβ), and YAP activation appeared to modulate stiffness-mediated signaling; when stiffness-mediated signals were blocked, collective MEC phenotypes were reduced in favor of single MECs migrating away from spheroids,” the authors penned. “These data indicate a more complex interplay of time-dependent stiffness signaling, spheroid structure, and soluble cues that regulate MEC plasticity than suggested by previous models.”
“In a dynamic environment, we found that these different pathways act cooperatively. It’s not enough to inhibit just one of those pathways as was previously shown in studies modeling static, stiff environments,” added Engler. “From a clinical perspective, this suggests that a single drug approach may not work for all patients with breast cancer tumors.”
Remarkably, the team also discovered that a subpopulation of mammary cells does not respond to stiffening. Engler says this is good news for women as fewer cells than previously thought may turn into cancer as a result of the environment alone. Such a result, if it translates to patients, could mean fewer or smaller primary tumors.
The investigators were energized by their findings and now plan to explore drug candidates to inhibit the pathways and study their effects on tumor progression. This research was done primarily on genetically controlled cell lines, so the team will follow up with studies on patient-derived cell lines.


