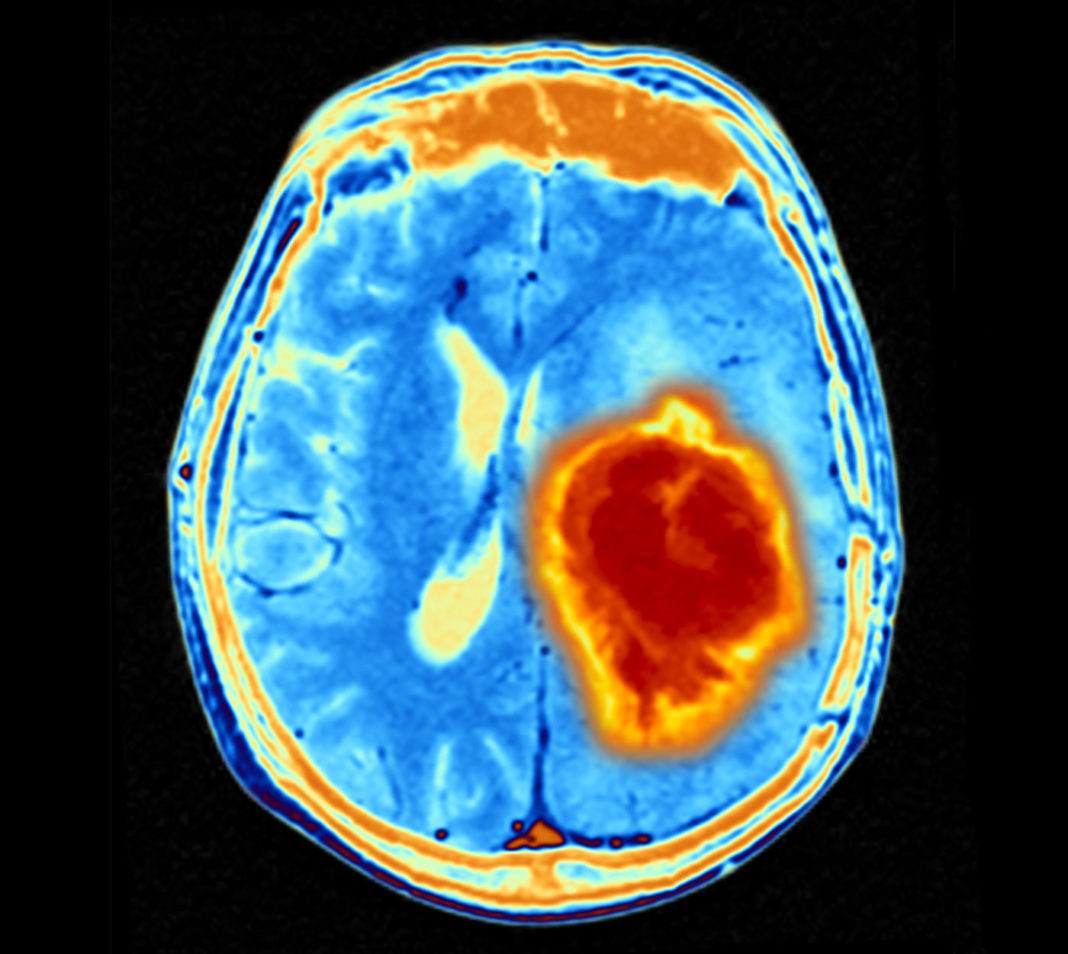
Researchers are seeking new ways to overcome the immune escape of glioblastoma cancer cells as they are able to adapt their identity to escape treatment. Now, new findings in mice by researchers at Cleveland Clinic reveal that glioblastoma cancer cells may use mitochondria from the central nervous system to grow and form more aggressive tumors.
The findings are published in Nature Cancer in an article titled, “GAP43-dependent mitochondria transfer from astrocytes enhances glioblastoma tumorigenicity.”
The research showed that it is common for healthy astrocytes to transfer the energy-producing organelles to glioblastoma cancer cells. When this process happens, it makes the cancer more deadly and the tumors more likely to grow.
“The transfer of intact mitochondria between heterogeneous cell types has been confirmed in various settings, including cancer,” wrote the researchers. “However, the functional implications of mitochondria transfer on tumor biology are poorly understood. Here we show that mitochondria transfer is a prevalent phenomenon in glioblastoma (GBM), the most frequent and malignant primary brain tumor. We identified horizontal mitochondria transfer from astrocytes as a mechanism that enhances tumorigenesis in GBM.”
“Defining the complex interactions glioblastoma cells have with the brain and nervous system is critical for developing new treatments for this highly aggressive form of brain cancer,” said Justin Lathia, PhD, staff in cardiovascular & metabolic sciences and the Melvin H. Burkhardt endowed chair for neuro-oncology clinical research. “We knew that this type of transfer was theoretically possible, but we didn’t know how relevant and dangerous it was in brain tumors.”
The study investigated mitochondria transfer in glioblastoma. Previous studies established that mitochondria transfer can also happen in other neurological conditions.
When cancer cells receive mitochondria, it affects the processes that produce energy. The study found in glioblastoma, this boost supports cancer stem cell properties including self-renewal and tumorigenicity, Lathia said.
“Cancer—and cancer treatment—does not exist in a vacuum,” Lathia added. “You’re not just treating and researching the tumors alone, instead tapping into a diverse ecosystem. Further research into this pathway can identify new strategies for treating glioblastoma, but also has potential for understanding other types of cancer.”