Precision medicines, such as cell therapies, remain expensive to manufacture and hard to access by patients. For example, Kymriah, the first chimeric antigen receptor (CAR) T-cell treatment approved in the United States, can have price tags as high as $475,000. Unfortunately, precision medicines are expensive to develop and manufacture, and the costs are ultimately borne by taxpayers and patients, according to “The State of Personalized/Precision Medicine” a report issued last year by GlobalData.
Today, companies are developing new models to lower the costs of manufacturing and bring drugs to more patients. Among them are companies developing new business models and services, innovative equipment for on-site manufacturing in hospitals, and improved formulation technology.
Reorganizing supply chains
A key challenge for companies is scaling up the delivery of precision medicines, notes Janel Firestein, partner and life sciences industry leader at Clarkston Consulting. Companies supplying precision medicines are harvesting material for patients in a hospital or clinic, and then freezing or shipping it fresh to a contract manufacturing organization (CMO), contract development and manufacturing organization (CDMO), or other manufacturing entity.
“What we’re seeing with a lot of our clients leveraging contract manufacturers is they’re contracting for specific slots,” she says. “They have x number of slots per week or month, and the scalability of that is hard.”
Precision medicines are manufactured in small batches in accordance with genetic, environmental, and lifestyle factors, that is, for patients in subpopulations that meet certain well-defined criteria. (The subset of precision medicines known as personalized medicines are even more specific; that is, they are developed uniquely for each individual patient.) If a patient doesn’t pass prescreening at the scheduled time, Firestein warns, the manufacturing slot for the patient’s treatment is lost unless the manufacturer can find another eligible patient.
Conversely, if the company is working across multiple CMOs in different countries, it needs to schedule slots in a predictable way. “You need to know which slots are open,” Firestein points out. “You need to leverage automation and artificial intelligence to give a manufacturing view to physicians at the patient hub, so they know which dates are available and can ensure the patient’s cells are viable upon receipt at the manufacturing plant.”
Bringing point-of-care processing to hospitals
Orgenesis is among the companies turning to localization to deliver precision medicines to patients. The company’s CEO and director, Vered Caplan, is a serial entrepreneur and among the top 20 inspirational leaders in advanced medicine listed in The Medicine Maker’s Power List 2020. Caplan has developed a point-of-care business model for hospitals that combines technological and biological development with a business strategy.
“We see that centralized processing is very costly,” she explains. “It can be a solution for companies working in clinical trials, but—once you get to market—it is not feasible for large numbers of patients.”
The company’s Cell & Gene Therapy Biotech Platform incorporates the following elements: POCare Therapeutics, a pipeline of licensed cell and gene therapies (CGTs); POCare Technologies, a suite of proprietary and in-licensed technologies; and POCare Network, a collaborative, international ecosystem of research institutes and hospitals. This platform, the company asserts, is about decentralization, enabling precision medicines to be prepared on-site at hospitals.
The platform automates the production of precision medicines by validating “closed box” processes to reduce cleanroom footprints once the product gets to market. Caplan works to develop and commercialize drugs that can be licensed for use by hospitals in the Orgenesis network.
“What we do is offer a low-cost supply platform with processing and regulatory solutions that are validated in a harmonized fashion,” she details. “Essentially, we take responsibility for R&D. Our hospitals are partners, and because we’re working in a network, the economic burden isn’t high, and we can supply the therapy at a reasonable cost.”
The Orgenesis approach doesn’t follow the usual approach, which involves a hospital research center licensing its drug to a pharmaceutical company, which then pays the center for clinical trials. Instead, Orgenesis works in partnership with a partner hospital throughout the commercialization process. Production of the final product is automated and supplied via an on-site point-of-care processing unit—reducing the complex logistics involved in transporting cells.
Taking production in-house
Fujifilm Diosynth Biotechnologies, a global CDMO, is developing a new platform to streamline the development of adeno-associated viruses (AAVs) for gene therapies. There are three methods to make AAVs, says Steve Pincus, PhD, the company’s head of science and innovation. Two of the methods use viral vectors, and a third uses plasmids.
“People using the latter need a source of cells and plasmids,” he notes. Unfortunately, there are few licensable cell lines and few plasmid manufacturers. Consequently, as Pincus points out, “If you want to manufacture your GMP plasmids at one of these, you have to wait 6 to 12 months to get in the queue.”
Fujifilm wanted to tackle these problems, so it decided to license five different Rep-Cap plasmids, an adenovirus helper plasmid, and a human embryonic kidney 293 (HEK293) cell line for AAV production by plasmid transfection from Oxford Genetics. Pincus explains that by licensing these technologies, the company means to offer an HEK293 master cell bank that is well characterized and stocks GMP-grade Rep-Cap and helper plasmids, so that “people can come and use those readily available reagents” without having “to wait 6 to 12 months,” and so that “the clients pay only for what they need.”
To support the production of AAVs, Pincus and his team are developing specialized upstream and downstream processes. They are also developing in-process analytics for common problems in the AAV manufacturing space, such as measuring empty and full virus capsids.
A machine for every patient
Earlier this year, on September 8, Lonza announced that in a project at Sheba Medical Center in Israel, the first cancer patient received a CAR T-cell therapy that had been manufactured using the company’s Cocoon® platform. Cocoon is another model for distributed manufacturing—a closed, automated piece of equipment for manufacturing cell therapies at the scale of a single patient, with a custom cassette that incorporates all the media, agents, and other consumables.

“When you look at the way cell therapies are manufactured, one of the costs is cleanroom space,” says Matthew Hewitt, PhD, head of clinical development and personalized medicine at Lonza. A cleanroom suite graded class B for air quality is noticeably more expensive than one graded class C, and the size of the room also matters. “If you move to a closed or functionally closed automated platform like the Cocoon that has integrated cell culture, then you can move to cheaper cleanroom space,” Hewitt asserts. “or you can increase the manufacturing density in your existing cleanroom to use the space more efficiently.”
Hewitt divides CAR T-cell manufacturing into a seven-step process: 1) collecting a patient sample; 2) preparing the sample for manufacturing; 3) activating the cells; 4) modifying (transducing) the cells; 5) expanding cell populations as needed for dosing; 6) washing, harvesting, and formulating the cells; and 7) dosing the patient. According to Hewitt, the steps currently automated by Cocoon include activation, transduction, and washing/harvesting/formulation. Additional automation features, he says, will debut in the coming months. Later this year, the company will begin beta testing automatic magnetic cell separation. Next year, the company plans to incorporate automated sample preparation into the Cocoon’s cassette.
Speaking on the future of manufacturing for precision medicine, Hewitt says he sees a role for both distributed and centralized models. Lonza’s centralized facility in Houston, TX, for example, can offer standardized and well-controlled conditions, as well as an experienced team, for process development and early-stage activities.
“Once you get to later stages,” he points out, “manufacturing needs to be moved toward the point of care to mitigate any issues with logistics.” He adds that as cell therapies become more common, building enough space to process patient therapies at a centralized facility becomes increasingly impractical. “Even if your centralized location served 50,000 patients a year,” he says, “the logistics would be a heroic endeavor.”
A film for formulation
“Gene and cell therapies don’t have much going on in terms of formulation,” says Maria Croyle, PhD, professor of molecular pharmaceutics and drug delivery at the University of Texas at Austin. “The formulation side needs to catch up.”
She argues that even though precision medicines are often formulated just by adding glycerol to the cells, preparing precision medicines to dose the patient is often a complex process. “When I talk about these therapies to my students,” she relates, “I explain that you need to thaw them out and do complicated dilutions. It’s not as simple as adding 5 mL to a flask.”
Precision medicines are often stored on-site in ultra-low-temperature (−80°C) freezers, devices that are, Croyle notes, expensive to run. The costs are often passed onto the patient. In addition, preparing the medications often involves lengthy dilution processes. Any of these medications that aren’t used within a couple of hours must be discarded, pushing costs yet higher.
Although some companies are moving to freeze-drying as a way to preserve living viruses and cells, preserving a live virus can take 48 to 72 hours. “I had no idea until I talked to industry how much freezer dryers were a power drain,” she recalls. “They use a lot of electricity for 72-plus hours, and that’s added to the cost of the drug.”
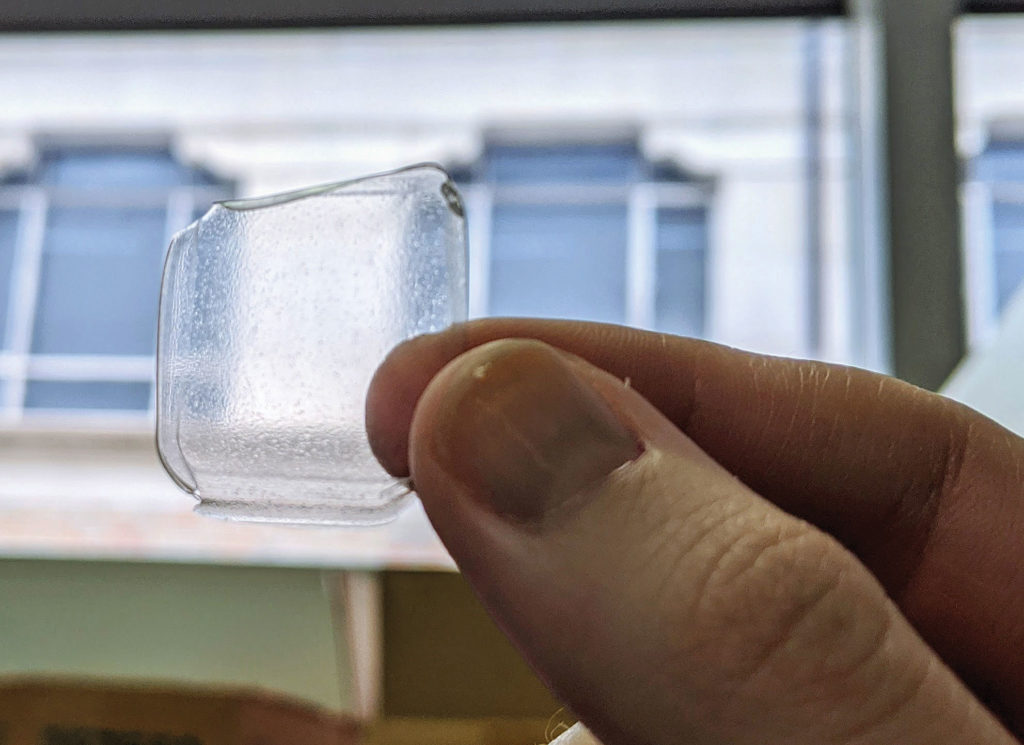
Croyle has developed a method for stabilizing live viruses inspired by the film Jurassic Park, which depicted the recovery of dinosaur DNA from amber. She has three patents on a peelable film, inspired by amber, into which gene therapy or vaccine products can be suspended and dried within hours. “You can mix them by 8 am, peel them by 3 pm, and package them to be sent off,” she asserts. “It’s very simple and space saving—it’s just a flat envelope with a strip of film, and it can be used in a variety of ways.”
Film-packaged doses, she says, can be rehydrated to produce nasal-sprayable vaccines or injectable gene therapy solutions, or they can be placed under the tongue and upper cheek, where dissolution of the film surface releases the vaccine, activating an immune response. To commercialize the technology, she has founded Jurata Thin Film. The company is named after a mythical Lithuanian goddess who lived in an amber castle under the sea.


