The handful of recently approved T-cell therapies should expect a lot of company soon. Many additional T-cell therapies are in the pipeline, marking one clinical trial success after another. The science works. But what about the economics? That’s a little less clear. Unfortunately, T-cell therapies will remain tantalizingly out of reach if they cannot be manufactured in a commercially sustainable way.
T-cell therapies pose serious manufacturing problems. In fact, as the science progresses, the problems seem to grow more varied. But manufacturing solutions are proliferating, too. Often, these solutions first appear at industry events, where conference programs are chock-full of presentations on topics such as cleanroom configurations, modular facilities, product expansion options, and co-culture technology. Many of these solutions are discussed in this article, which means to disseminate the most interesting proposals for improving T-cell manufacturing.
Planning ahead
Should we use a contract manufacturing organization (CMO) or keep manufacturing in-house? How big should the facility be? What should it look like? Questions such as these confront companies large and small.

Chief Technology Officer
Mustang Bio
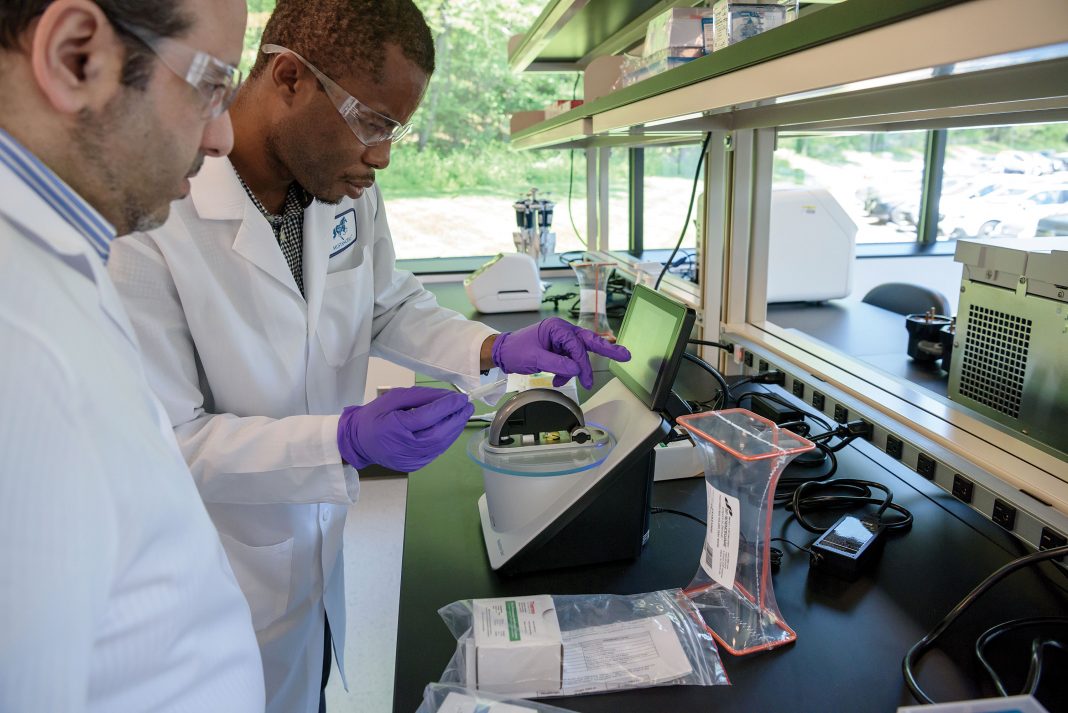
“More and more relatively small companies like ours are building out their own manufacturing facilities,” says Knut Niss, PhD, chief technology officer at Mustang Bio. “Five years ago, nobody had done that.” The manufacturing facility, the infrastructure, the personnel—these are major drivers of the cost of goods in cellular therapies. Consequently, an efficient facility—one that has a higher capacity and a smaller footprint—can help reduce cost of goods.
It’s never too early in clinical development to think about what a commercial facility should look like, and to start designing your facility accordingly. “If your clinical development is successful, you will be much faster to market if you don’t have to go back and redesign your facility,” Niss explains. “Things can move very quickly, especially in cell therapy. Making changes can be very hard.”
Think about where you are now and whether you are confident your product will reach the market, Niss advises. Also, he suggests that you ask what might happen to your facility if your product fails. “If you build a facility for chimeric antigen receptor (CAR) T-cell processing, you will always find somebody who has an interest in using that facility,” Niss argues. “Manufacturing capacity in the field is so limited.”
Niss shared some of the planning and experiences involved in the multiphase buildout of Mustang Bio’s new CAR T-cell facility when he addressed his audience at the August 2019 Bioprocessing Summit in Boston. The facility started out incorporating very generic 3000–4000-square-foot cleanrooms, to provide flexibility in case the company’s initial plans didn’t work out. Over time, the company grew more certain of its approach.
“We are in deeper and very confident about our assets,” Niss declares. “We are building out the next phase in a more cell processing–specific way.”
At bench or pilot scales, unit operations require little space, simplifying the interconnection of whatever equipment is involved. However, in a commercial setting, different unit operations cannot occupy the same space. “You need to have unidirectional flow,” Niss points out. “Cells spend at least 95% of their time in closed containers in an incubator.”
A commercial-scale facility, such as the one Mustang Bio is currently designing and building, may boast multiple small cleanrooms, each with a separate entrance and exit. Specially designed incubators—with a small footprint, to hold the cells of a single patient—may be placed in a corridor, freeing up space in the cleanrooms.
Niss expects that the Mustang Bio facility will house at least 160 incubators and accommodate 3000–4000 CAR T-cell processes per year. Once the facility reaches its full extent—about 14,000 square feet—it will have about 1/10th the footprint of currently existing plants. And by designing the facility to meet both U.S. and European standards, Mustang Bio is prepared, Niss says, to “more or less double” capacity and serve both U.S. and European markets without having to build and manage a new facility in Europe.
Keeping it simple
Over the past decade, Memorial Sloan Kettering Cancer Center (MSKCC) has manufactured hundreds of patient-specific CAR T-cell products, for 13 early-phase clinical trials covering different disease applications. MSKCC used modular unit operations for each of the processes involved including T-cell stimulation, viral transduction, washing, and incubation.
“I think we are at the stage where we know what we are doing,” says Xiuyan Wang, PhD, assistant director of MSKCC’s Michael G. Harris Cell Therapy and Cell Engineering Facility. “We have a set procedure.”
Wang and her colleagues have become familiar with the CliniMACS Prodigy, an automated cell manufacturing platform developed by Miltenyi Biotec. According to Wang, the MSKCC team started by evaluating how the platform “incorporates all steps of the manufacturing process from T-cell selection to end-of-process CAR T-cell formulation,” and how it compares to a modular platform. At the time this article was written, she planned to share her team’s findings at a September 2019 conference, Cell and Gene Therapy Bioprocessing and Commercialization, part of Biotech Week Boston.
In their work with the Prodigy platform and the modular platform, Wang and colleagues ensured that the processing procedures were as identical as was feasible, with the principle difference being that magnetic Dynabeads were used to stimulate cells in the modular platform, whereas in the Prodigy, biodegradable TransAct beads were used.
The resulting products were introduced into both prostate cancer and leukemia mouse models. The MSKCC team noticed that the products coming out from the Prodigy platform appeared to be “a little bit more potent,” Wang reports. “We did some cellular immunology type of studies, mainly FACS, to look at the phenotype of the cells. Prodigy-produced cells had higher antitumor activity, with a more central memory phenotype.”
A modular platform offers flexibility—in reagents, equipment, and protocol—for people doing more innovative work, especially in an academic setting, but requires well-trained technicians. “For established protocols, where people know exactly what they want to do, and the procedure won’t be adjusted too much, Prodigy does have the advantage of less variability between operators,” Wang notes. “It’s more uniform. It’s less likely to allow contamination. It’s a closed system. So, Prodigy may be easier.”
According to Wang, both Prodigy and the modular platform can generate cells to support clinical trials, even late-stage clinical trials. She suggests that the Prodigy could be especially useful to newer companies, which may lack technical expertise. “If they have the upfront capital for the Prodigy,” she says, “they may be able to go online more quickly.”
Stirring the pot
“The platforms that are being used to manufacture cell and gene therapies are inherently expensive,” comments Qasim Rafiq, PhD, associate professor of biochemical engineering at University College London. He adds that the healthcare system cannot be expected to pay for these therapies—not when the cost per patient is $300,000. The high cost is due to several factors including lack of process understanding, labor intensiveness, and the need for facilities to accommodate open processes by installing cleanrooms. “One way to reduce the cost of therapies,” Rafiq suggests, “is to reduce the cost of manufacture … by moving toward closed, scalable, automated platforms.”
Manufacturers of cell and gene therapies might consider transitioning to stirred-tank bioreactors. They have long served as the workhorses of the biologics industry. “We understand them,” says Rafiq. “They’re regulated, and many companies have the existing infrastructure and capability in-house.”
Yet T cells are traditionally grown in static environments such as T flasks and bags—which are not scalable and lack fundamental process monitoring and control capability. Stirred-tank bioreactors have been avoided largely because of fears that agitation may induce sheer stress. These fears may be unfounded, Rafiq suggests.
At the time this article was written, Rafiq planned to make his case at the Cell and Gene Therapy Bioprocessing and Commercialization conference. He intended to present evidence that primary T cells and CAR T cells have been grown in an ambr® 250 single-use stirred-type bioreactor vessel. Using this platform, which was developed by Sartorius Stedim Biotech, Rafiq and colleagues experimented with different agitation rates.
“We’ve shown not only that relatively high agitation rates do not damage the cells, but also that better growth may be achieved,” Rafiq states. “That’s as a result of the improved mixing conditions for both the Dynabeads, which activate the T cells, as well as improved mass transfers” of oxygen, glucose, and other key nutrients and metabolites. The system enables the process to be extensively monitored and controlled.
The platform can be fully automated and scaled out, allowing up to 24 completely self-contained bioreactors to be simultaneously controlled in parallel. It can also serve as a scale-down model for process development and optimization, for example, for growing large amounts of product for allogeneic (universal) T-cell therapy.
Co-culturing different cell types
In the next generation of T-cell cancer therapies, the T cells will have a library of molecules on their surfaces, and these molecules will recognize and target tumor-specific neoantigens. Bespoke T-cell therapies will be generated by selecting the patient’s own T cells against libraries of neoantigens. After the neoantigens are acquired by sequencing the tumor, they will be presented by the patient’s own dendritic cells (DCs). Because DCs are not abundant in circulating blood, they are typically prepared by first differentiating them from monocytes.
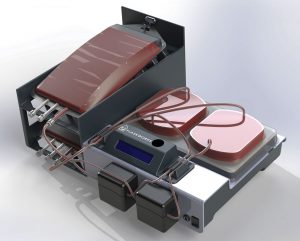
DCs and T cells may be co-cultured, but suitable instrumentation is required, says Shashi Murthy, PhD, professor of chemical engineering at Northeastern University. At the time this article was written he was scheduled to describe the design of such instrumentation at the Cell and Gene Therapy Bioprocessing and Commercialization conference.
“DCs so generated are adherent cells, and T cells are suspension cells,” Murthy explains. “So, you have to design a bioprocess to generate adherent cells and then be able to co-culture that adherent cell type with a suspension cell type.
“At the end of that process, you’re recovering the suspension cell type only. Further adding to the complication is the fact that this type of stimulation will sometimes need to be done in multiple cycles, [requiring] a fresh supply of DCs that are stimulated with a different batch of antigens.”
To keep T cells happy, instrumentation may incorporate a polystyrene-bottomed surface for optimized generation of DCs; a perfusion apparatus consisting of a tubing set; and a vessel with adequate headspace and perfusion-mediated gas exchange. “It’s sort of a hybrid between static vessels and gas-permeable bags,” Murthy says. “It’s all a closed system.”
According to Murthy, fully integrated automated systems are very capable but too expensive to adopt at the preclinical stage. “A lot of work is done manually and then translated into such systems,” he notes. “Now there’s a move in the industry to try to build closed systems that are sufficiently robust for clinical manufacturing and provide the benefits of automation, but at the same time are affordable enough to integrate into preclinical and Phase I environments.”