June 1, 2016 (Vol. 36, No. 11)
Clinicians Need to Understand Genetic Tests Quickly and in Clinical Context
With $215 million in funding, the federal government’s Precision Medicine Initiative® is expected to generate the scientific evidence needed to move personalized medicine into clinical practice by providing clinicians with the knowledge and tools to determine more precise medical treatment.
One objective of the initiative is to accelerate pharmacogenomics (PGx), which assesses an individual’s unique genomic markers to predict how they will respond to a specific drug in order to help clinicians more closely tailor personalized treatment, and choose safer and more effective therapies.
PGx testing is also important toward identifying gene variations that cause adverse drug reactions, currently estimated by the Food and Drug Administration to cost the U.S. more than $136 billion per year.
Complex Data Overwhelms Cognition
PGx testing provides tremendous clinical value, but the data is nearly useless without proper clinical context. Genetic data is extremely complex, involving the interactions of up to 200 variations of approximately 30 genes that have actionable data for 200 drugs or so. The growing volume of available genetic diagnostic tests, currently estimated to be more that 33,500 at the National Center for Biotechnology Information’s genetic testing registry, makes it challenging for physicians to keep current or manually assess all the co-determinants for an appropriate course of therapy.
With increasingly larger assays, whole ‘ome sequencing, and results that are relevant for multiple purposes, the challenge of translating from molecules to medicine intensifies, and evaluating clinical evidence requires expert curation. It is not just a matter of looking up a gene mutation to determine how a patient will metabolize or react to a given drug. There is a wide range in evidence quality, and many gaps exist in the data and variant databases.
Not all genotypes are straightforward; it is difficult to infer structural variation, and data analysis consumes a great deal of time and expense. Ironically, the large amount of raw, non-actionable data generated by genetic testing, and the challenge to give the data meaning, may actually lower a clinician’s propensity to use genetic tests to advance precision medicine.
Many electronic health record, laboratory, drug interaction checking, and prescribing systems do not incorporate or leverage genetic information, or cannot accurately evaluate cumulative drug-drug-gene variations to help clinicians predict potential interactions and adverse drug events when choosing alternative patient therapies. Another factor complicating the interpretation of genomic data is the often lengthy, overly detailed, complicated reports that do not effectively guide decision making.
Clinical Decision Support Systems
To gain the benefit of precision medicine, clinicians must be able to understand the implications of genetic tests quickly using drug-drug-gene-based clinical decision support and reporting tools. To be used efficiently in daily practice, solutions must be integrated into the prescribing process, building on concepts and systems that are already familiar and part of the existing physician workflow.
A clinical decision support solution from Translational Software, Inc. (TSI) provides access to a continually updated PGx knowledge base that guides when a genetic test is indicated, interprets raw genetic test results, and converts the findings into actionable reports that highlight which drugs are relevant, what genes affect those drugs, whether there is risk for an adverse drug event, and which SNPs should be tested for the highest impact at least cost.
Reports incorporate the latest guidance from leading-edge science, knowledge from scientific groups such as the Clinical Pharmacogenetics Implementation Consortium and the Dutch Pharmacogenetics Working Group, and government data from the Federal Drug Administration and the European Medicines Agency as well as other primary sources.
This molecular intelligence is integrated along with the patient’s history and organizational-specific testing policies to provide the right information and context within the clinical workflow as part of the laboratory information system, electronic health record, or other prescribing system.
Visual, Decision-Ready Reports Are Key
To truly guide clinical decision making, genetic interpretation reports must be succinct, and quickly highlight the priority information that is most critical to patient care. Visual aids, including flags, alerts, and strategic use of color, are essential to help clinicians understand and weigh important treatment trade-offs (Figure). It is important that alerts focus on the consequences, not the genetic result. Reports also need to be customized for the recipient based on clinical context, and tailored to the clinician’s specific medical discipline.
TSI’s reports provide a color-coded list of all known medications for which dosing should be personalized based on the patient’s genetic test results, coupled with recommended medication alternatives and dosing guidance. Each report contains current patient medications, complete PGx results, potentially impacted medications, dosing guidance, genetic test details, drug-drug-gene interaction risks, and a patient summary. Reports link to the most recent drug labels and approval history with quality-assessed, systemic reviews of drug safety and efficacy.
With interpretation for nearly 40 genes, TSI’s platform can be tailored to a variety of clinical specialties including cardiovascular, psychiatric, pain, and cancer.
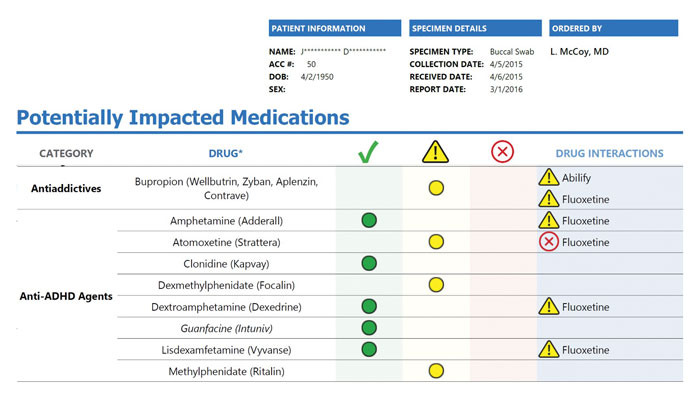
Figure. TSI’s reports allow clinicians to quickly visualize trade-offs between medications given the patient’s PGx results and known drug-drug interactions.
Real World Implications—PGx in Practice
Inova Women’s Hospital in Falls Church, VA offers an optional one-time pharmacogenomic test called MediMap™ that evaluates 7 actionable genes associated with more than 21 drugs to determine how a baby will uniquely respond to certain prescription medications. TSI has partnered with Inova to interpret the raw genetic data and generate a tailored report for each newborn that provides molecular intelligence and critical alerts regarding drug efficacy, toxicity, and known interactions.
“Having an advance understanding of a newborn’s genetic makeup and response to commonly prescribed medications gives our physicians a tool to help personalize treatments for life, and helps Inova practice genomic medicine in real time,” said Benjamin Solomon, M.D., Chief, Division of Medical Genomics at Inova Translational Medicine Institute.
It is anticipated that testing every patient’s genetic code may someday be routine to help guide treatment decisions for life. Toward this end, the PGx results of a single genetic test may be used for many purposes, across numerous treatment episodes in a patient’s lifetime. Concise PGx reports need to be part of a permanent electronic health record for this purpose.
By leveraging technology to help capture, interpret, and share PGx data, clinicians can make better decisions about care delivery with the goal of enhancing the patient experience, improving quality and outcomes, and reducing the costs of healthcare. Ensuring that concise PGx results interpretation and reporting is the primary product of genetic testing and not just an afterthought is central to advancing precision medicine initiatives.
Don Rule ([email protected]) is CEO and Houda Hachad, Ph.D., is CSO at Translational Software.



