The global issue of antimicrobial resistance has been called a “slow motion catastrophe” resulting from the excessive and often inappropriate use of antibiotics to fight bacterial infections.1 A long-standing unmet need is the availability of a quick and easy clinical test to support a more evidence-based approach to the use of antibiotics.
Although antimicrobial susceptibility testing (AST) represents the standard of care for treating bacterial infections, current methods2 can be slow and laborious. An AST can be either a genotypic or phenotypic test, yet the latter is the preferred reference utilized worldwide.
The most common phenotypic AST testing methods are either a broth microdilution (BMD) or a disc diffusion assay. However, the internationally accepted standard for AST uses a specific version of the BMD that provides a semi-quantitative measure of antimicrobial resistance known as minimum inhibitory concentration (MIC) for the tested antibiotic.3 To perform this test, bacterial cultures are grown with dilutions of antibiotic and are quantitated in terms of MIC, the lowest antibiotic concentration (µg/mL) that inhibits bacterial growth. However, the process can take from six to 24 hours or more.
Spencer and colleagues4 describe a rapid, label-free phenotypic AST, termed iFAST, which can provide a resistance profile in as little as 30 minutes. This high-throughput test measures changes in the electrical and morphological properties in solution of thousands of single bacteria using microfluidic impedance cytometry.
Senior author of the paper, Hywel Morgan, PhD, professor of bioelectronics in the School of Electronics and Computer Science, and Institute for Life Sciences, University of Southampton, U.K., says, “The technique involves measuring the electrical properties of bacteria to look for changes induced by the antibiotic. While this has been done in the past, the emphasis has been on looking for changes in the properties of the media. We examine the changes in individual bacteria which surprisingly become visible after only 30 minutes exposure.”
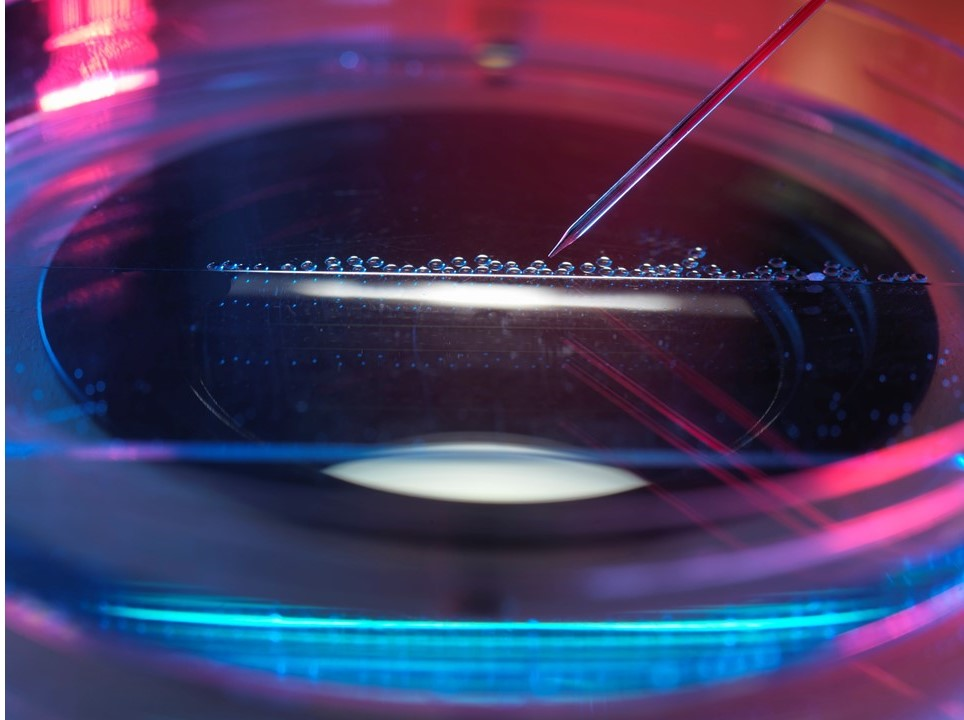
Morgan says that the basic method incubates a bacterial sample with various concentrations of the antibiotic for about an hour followed by immediate sample analysis. To do this, the cells are guided through a small channel in a microfluidic chip. Inside this channel are small electrodes roughly the size of bacteria. Cells pass one by one between the electrodes.
“We can measure about 50,000 bacteria in a few minutes. To get a data readout, we compare unexposed bacteria with bacteria exposed to the antibiotic,” reports Morgan.
Microfluidic impedance cytometry has been broadly employed for the label-free characterization of mammalian cells.4 In this case, the electrical impedance signal indicates changes in the electrical properties of bacteria.
Morgan notes, “It provides a value of the volume of the organism (which changes when exposed to antibiotics), the cell wall properties (permeability, that depends on cell viability), and the internal properties of the organism. It is very simple and requires no reagents and is performed with bacteria suspended in their native environment, i.e., growth media.”
Although the new method works well in a laboratory setting, can it translate to the clinical laboratory? Morgan states, “The test is absolutely suited to a clinical laboratory and has been designed to integrate seamlessly into the standard workflow. The bacteria are incubated in a simple disposable plastic cartridge. For all the bacteria and antibiotics measured so far, the test results map extremely well to the current broth microdilution test, which takes 24 hours.”
Morgan and colleagues are currently working to build a library of data using clinical isolates of bacteria and clinical samples tested with a spectrum of front-line antibiotics. As to the future, he notes, “We are now setting up a company to commercialize the technology. Our aim is to develop the first test cartridge with a focus on two areas where urgent intervention is required, namely, urinary tract infection and sepsis.”
References
- Lesho EP, Laguio-Vila M. The Slow-Motion Catastrophe of Antimicrobial Resistance and Practical Interventions for All Prescribers. Mayo Clin Proc. 2019;94(6):1040-7.
2. Henderson A, Bursle E, Stewart A, Harris PNA, Paterson D, Chatfield MD, et al. A systematic review of antimicrobial susceptibility testing as a tool in clinical trials assessing antimicrobials against infections due to gram-negative pathogens. Clin Microbiol Infect. 2021;27(12):1746-53.
3. Spencer DC, Paton TF, Mulroney KT, Inglis TJJ, Sutton JM, Morgan H. A fast impedance-based antimicrobial susceptibility test. Nat Commun. 2020;11(1):5328.
4. Chen J, Xue C, Zhao Y, Chen D, Wu MH, Wang J. Microfluidic impedance flow cytometry enabling high-throughput single-cell electrical property characterization. Int J. Mol Sci. 2015;16(5):9804-30.